Recommended
Please note this blog is part of a short series on COVID-19 and mortality. Please see here for our previous blog “What Matters Most for COVID-19 Policy Now: Better Mortality Data” and here for a link to the event.
What is the true death toll of the COVID-19 pandemic? We don’t know, but there is consensus on one thing: the numbers are likely worse than official figures show.
The adage “better data drive better decisions” could not be more true in the current context. Countries need both accurate and timely mortality data and an understanding of the scope and scale of the pandemic in real-time to inform a data-driven response. What we are seeing today—and what experts have known for some time—is that many countries lack this data, which is reflective of a longstanding underinvestment in civil registration and vital statistics (CRVS) systems.
To respond to COVID-19 in the near-term and bolster global health security in the long-term, it is clear: we need better mortality data.
Recognizing this urgency, CGD brought together experts to discuss progress, obstacles, and new directions for tracking mortality. CGD hosted an online event to discuss one approach, rapid mortality surveillance in low- and middle-income countries, as well as CRVS systems more broadly amidst COVID-19 and beyond. Here are three key takeaways on the current state of tracking mortality in low- and middle-income countries:
Estimates of excess mortality are useful but fall short when there are data gaps
Excess mortality has become a popular approach for measuring the impact of the COVID-19 pandemic. The measure, though useful in determining the toll of COVID-19 in countries with relatively robust CRVS systems, is less feasible in many low- and middle-income countries because underlying data systems have unreliable mortality figures and cause-of-death attribution. To overcome this problem, Philip Setel, vice president of CRVS at Vital Strategies, shared one strategy: rapid mortality surveillance (RMS), a tool that uses existing public data to triangulate information on total deaths from multiple sources including civil registration, burial data, and others, and is currently being used in 13 countries globally.
Brazil, one of the countries hardest hit by the COVID-19 pandemic, has used the RMS approach to compile data from both health system and civil registry in Brazil. Fatima Marinho, senior technical advisor of CRVS at Vital Strategies in Brazil, and colleagues created an excess mortality dashboard that has been used by decision makers and technical personnel to get a grasp of the pandemic’s impact in Brazil. Looking at disaggregated data by region through RMS allows us to see differences in mortality rates since the onset of the pandemic—an increase of over 18,000 deaths in the most populous state, São Paulo, and a 74 percent rise in mortality in Amazonas State—and is important for ensuring that policy responses adequately consider equity.
Participants agreed, however, that RMS and other fixes to tracking mortality are no replacement for sustainable, well-functioning CRVS and cause-of-death data systems.
Efforts to track mortality are numerous, but fragmented and limited in scale
Ongoing efforts lack coordination, not only between national health systems and civil registration systems—which sit in different ministries—but also between governments and communities, and across multilateral institutions and regional partners. Existing funding for CRVS often comes from “vertical,” disease- or condition-specific funding, which is both fragmented and at an insufficient scale.
The COVID-19 pandemic has shown the need for harmonized and timely efforts to bolster mortality tracking and CRVS systems. Samira Asma, assistant director-general for the Data, Analytics, and Delivery for Impact Division at the World Health Organization (WHO), called for partners to coordinate their efforts. We need to commit to common standards across actors, she said, “so we don’t keep reinventing the wheel.”
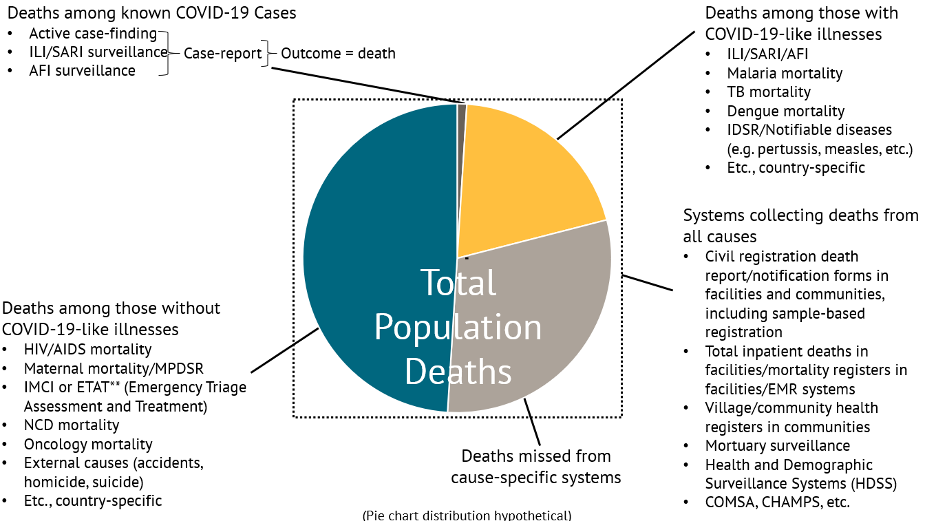
Erin Nichols, epidemiologist with the global CRVS team at the US Centers for Disease Control and Prevention (CDC) National Center for Health Statistics, pointed to a problem with numerous potential sources of mortality data across platforms: a significant proportion of deaths are missed by siloed systems and activities. More deliberate coordination and interoperability across actors and organizations collecting this information is necessary to bring information together in a useful and efficient way.
Sources of Mortality Data
Adapted from Erin Nichols’ presentation at CGD’s event, “Tracking Mortality Amidst COVID-19 and Beyond – Progress, Obstacles, and New Directions,” September 25, 2020 (Diagram by Emily Cercone, CDC Foundation)
Note: [ILI (Influenza-like Illness), SARI (Severe Acute Respiratory Illness), AFI (Acute Febrile Illness), IMCI (Integrated Management of Childhood Illness), NCD (Noncommunicable Disease), TB (Tuberculosis), IDSR (Integrated Disease Surveillance and Response), EMR (Electronic Medical Record), HDSS (Health and Demographic Surveillance System), COMSA (Countrywide Mortality Surveillance for Action), CHAMPS (Child Health and Mortality Prevention Surveillance)]
We need to keep attention on CRVS as the bedrock of global health security
COVID-19 has spurred momentum to improve mortality surveillance and CRVS systems, an area that, along with health systems strengthening, has been historically underfinanced. But it will be vital to avoid succumbing to the pattern of “panic and neglect” and maintain the focus far beyond the pandemic to achieve broader system-wide change.
To speed progress, an idea one of us (Glassman) and other collaborators have proposed is launching a Global Health Security Challenge Fund, a multilateral effort to incentivize low- and middle-income countries to invest domestic resources in filling critical preparedness gaps. Such an effort should be laser-focused on improvements in surveillance and CRVS.
Currently, the WHO is revamping its global mortality database, the CDC is supporting efforts to “coordinate, de-duplicate, and integrate” health information systems (Nichols), and Bloomberg Philanthropies’ Data for Health initiative is bringing together Vital Strategies, WHO, CDC, and other partners to improve data. This momentum should not be stalled.
Strengthening efforts and increasing investments in CRVS systems and mortality tracking will be useful not only for COVID-19 mortality surveillance, but also for creating more resilient health systems and must be a key focus of global health security going forward.
Disclaimer
CGD blog posts reflect the views of the authors, drawing on prior research and experience in their areas of expertise. CGD is a nonpartisan, independent organization and does not take institutional positions.
Image credit for social media/web: Simone D. McCourtie / World Bank