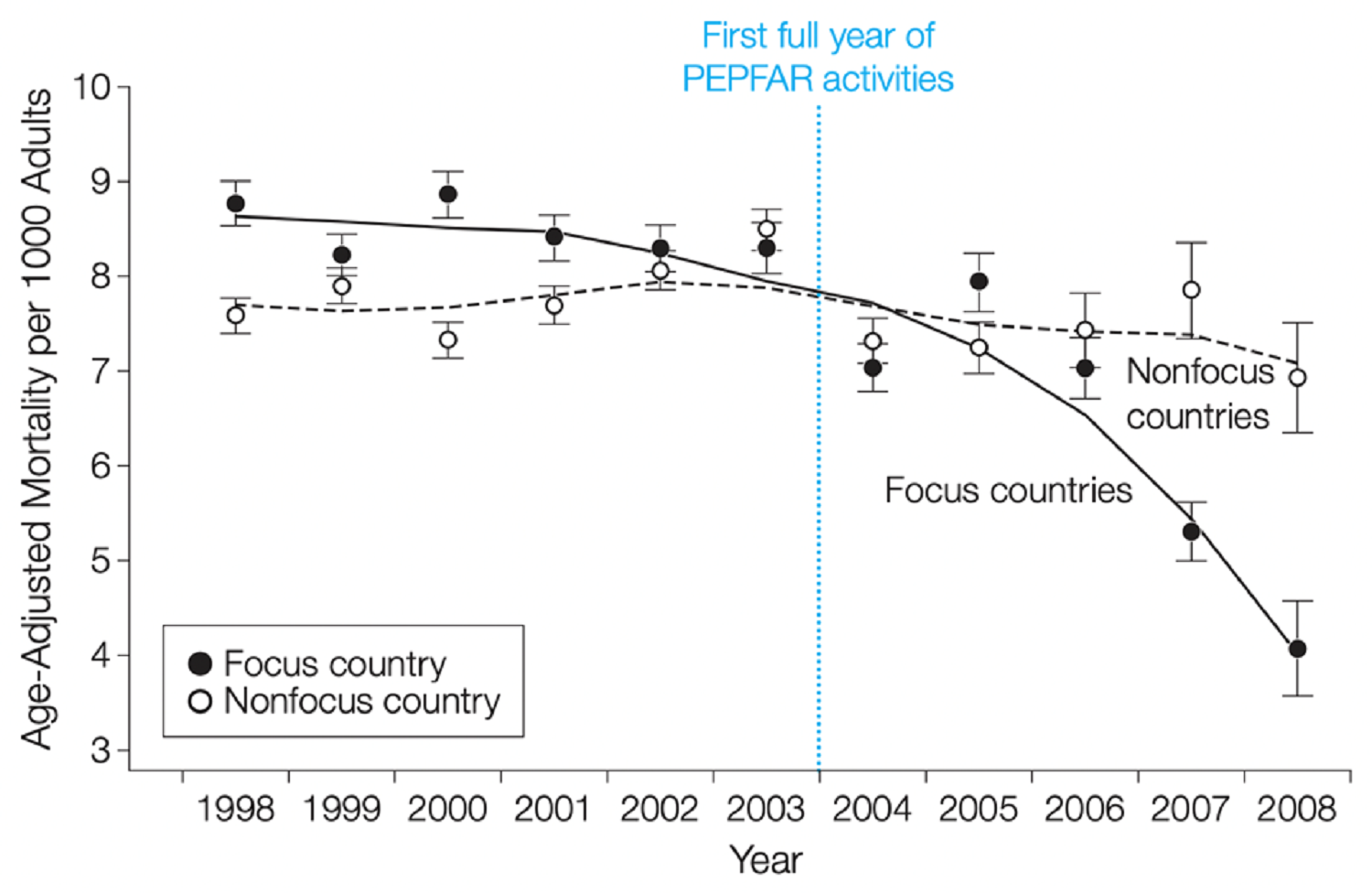
It’s entirely possible that the Obama administration will institute better global health policies than its predecessor, and appear to get worse results. This paradox, although painful, is all too easy to imagine.Take HIV/AIDS. Since President Bush announced the President’s Emergency Plan for AIDS Relief in the 2003 State of the Union Address, U.S. dollars have been put to work to get more than 2 million people started on antiretroviral treatment, most of them under the auspices of programs operated by U.S.-based contractors. PEPFAR has been hailed as a success, and can certainly claim credit for sparing many from certain death – at least while the ARVs are available and effective.The new administration, in part backed up by last year’s legislation reauthorizing PEPFAR, is addressing a host of critiques of the program by introducing new policies and practices: More attention to prevention, with reduced emphasis on the “abstinence” and “be faithful” programming. Use of resources to strengthen core functions of health systems, instead of establishing AIDS-specific supply chains and information systems. Alignment of spending with national priorities, and channeling an increasing share of the resources through national governments and local organizations, rather than through contractors. All welcome developments, consistent with recommendations that my colleagues who work on the HIV/AIDS Monitor have generated from several studies.Sadly, the potential benefits of these new policies may be preempted by cold, hard reality. Simply sustaining the current level of ARV coverage is challenging enough as budgets are squeezed, but the current level is going to look less and less impressive as more people become HIV+ and as pressures rise to expand treatment. (My colleague Mead Over has discussed this and related issues here and here.) Moreover, those who have been on ARVs for four or more years may start to fail treatment, further raising costs and attenuating the success of PEPFAR I.Improvements on the prevention side, which very well may result from smart policy and programmatic measures, will be awfully hard to detect. And while alignment with national governments and partnership with local organizations are undoubtedly positive developments over the long term, the risk of slow implementation, political capture, and reduced Congressional support are real threats to the “PEPFAR’s a big success” story.The President’s Malaria Initiative, a newer global health initiative, also has to figure out how to succeed after the start-up phase, particularly in the face of resources that are unlikely to grow proportional to the need. In Zanzibar, for example, where PMI has successfully collaborated with the government to bring about a decrease of more than 90 percent in malaria in children under 2, PMI is in the tricky position of having to figure out whether to move resources to higher-prevalence countries and document some impressive impacts – admittedly a tempting thing to do – or use them to maintain the achievements. If PMI moves the emphasis away from Zanzibar, malaria almost inevitably will roar back, just as it has done the two prior times the disease has been eliminated from the island, in the 1950s and 1980s. The right policy, and presumably the one PMI will choose, is to stay the course. But there will be a steep price: Gains under this phase of PMI will look markedly less impressive than those reported earlier.Finally, will the Obama Administration’s emphasis beyond HIV/AIDS and malaria, to maternal and child health and health systems, yield positive results? While details are yet to emerge, the language we’re hearing of integration and country-ownership – music to the ears of many of us – are by no means synonyms for better health fast. In addition, if strengthening health systems includes improving the ability to measure ill health and its risk factors, the numbers may start to look worse, simply as a reporting artifact.There is no clear-cut solution for these problems. But several actions could be taken. First, on the malaria and HIV/AIDS fronts, the key will be to construct and make public the right counterfactual now – that is, playing out scenarios about how the diseases would have played out under alternative policies and corresponding epidemiologic trends. In the end, just as for the TARP funds and stimulus package, the entire discussion about “success” or “failure” will hinge on what people believe about what would have happened in the absence of those policy measures. For diseases where the hard-to-see prevention stories could be dominated by the easy-to-see failures, building out the counterfactual is likely to be quite helpful – and doing it sooner rather than later will make it more like science and less like reverse engineering to get a predetermined answer.Second, on the MCH / health systems questions, there is tremendous potential to use approaches that link funding to results, within a framework that is negotiated with and aligned with national priorities. This is a long way of saying: performance incentives of various types hold a lot of promise. They represent a way to obtain improvements in health outcomes while at the same time giving local actors the latitude and resources they can use to reinforce elements of the health system. Performance incentives are already being used in innovative ways related to maternal and child health within a World Bank Trust Fund on Results-based Financing (which has pulled together many useful materials here).Third, devote part of the global health efforts to key challenges above the country level. One area in which most would agree the Bush administration had a track record that can be easily improved upon was in working cooperatively within the UN and other multilateral frameworks. Expectations are high that the current administration will do better, but participation in international meetings, declarations about harmonization, and “we’re all in this together” language is not enough. Better would be engaging in shared leadership on an international health initiative. The list of possibilities is long indeed. A few examples: An innovative financing mechanism for global health R&D. A greatly ramped up international system for drug resistance surveillance and information-sharing. A supranational contingency fund to partially protect countries from the economic costs of disclosing outbreaks of infectious disease. Any one of these, or a similar “global public goods” effort, would make a real and lasting contribution while diversifying the portfolio of U.S. investments in global health.
Disclaimer
CGD blog posts reflect the views of the authors, drawing on prior research and experience in their areas of expertise. CGD is a nonpartisan, independent organization and does not take institutional positions.