Recommended
Countries across the world, including the very poorest, have begun to implement heavy-handed measures to slow the rate of transmission of COVID-19. Even before taking those measures, low-income countries with hardly any identified cases were already reporting sizeable economic impacts. Travel and tourism have ground to a halt, producers can’t get materials, and retailers can’t get products. Global growth estimates are down, along with growth estimates for Africa, Latin America, and elsewhere. One estimate suggests that a 1 percent lower growth in the global economy would translate to between 14 million and 22 million more people living in extreme poverty.
But are the actions that we are taking in the United States and other high-income countries the same ones that should be implemented in low-income countries?
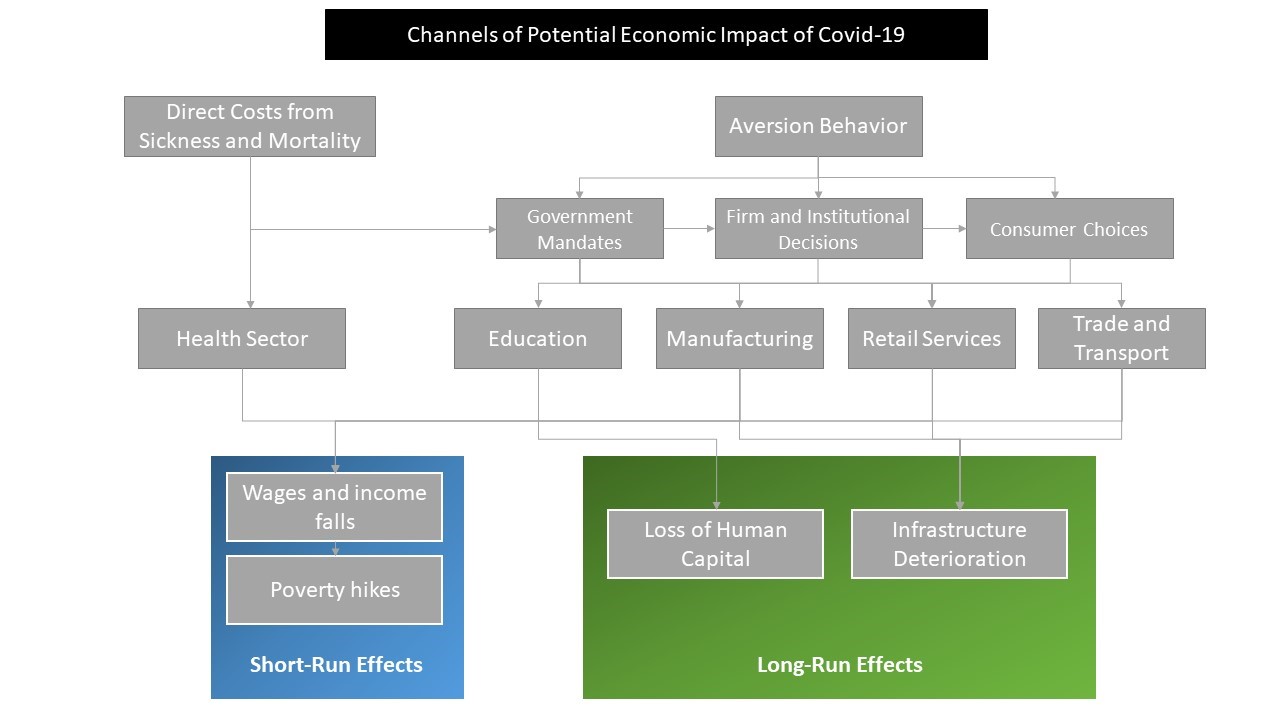
Stemming the spread of the disease and mitigating the impact on the economy are interwoven. As the disease spreads, it affects the economy with workers sick, caring for family members, and dying. As the economy slows, increased poverty means more deaths from hunger and other health conditions. Some actions to slow the spread of the virus are injurious to the economy, and some actions to revitalize the economy will make it harder to slow the spread of the virus. Any reaction must incorporate both health and economic risks. Expanding the safety net for poor households may be good for both, but the poorest countries also tend to have the weakest safety nets.
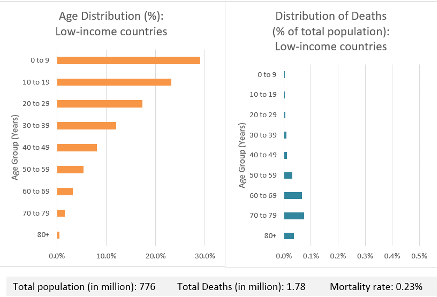
Low-income countries also differ from high-income countries in that they have far fewer elderly citizens, and COVID-19 is not affecting all segments of the population equally. Older individuals are much more likely to be affected, with the Imperial College COVID-19 Response Team reporting that symptomatic individuals in their seventies are twenty times more likely to require hospitalization than those in their twenties. What this means is that an uncontrolled virus could have a far lesser death toll in a much younger population. Consider Uganda and Spain, two countries with a similar total population size (between 40 and 50 million people) but with dramatically different age distributions of that population. In Uganda, more than half the population is under the age of 20 and only about one percent of the population is over the age of 70. In Spain, less than 20 percent of the population is under the age of 20, and 15 percent is over the age of 70.
Let’s pause for some assumptions. We’ll use numbers from the Imperial College report: absent measures to stem the rate of infection, 81 percent of a country’s population will get infected, 55 percent of cases will be symptomatic, and we retain the report’s age distribution of symptomatic cases requiring hospitalization and hospitalized cases requiring critical care from that report. Let’s add the dramatic assumption that all patients in critical care would tragically pass away. While this is not the case in high-income countries, many low-income countries have very limited critical care facilities, so it may not be as far from the truth as we’d like.
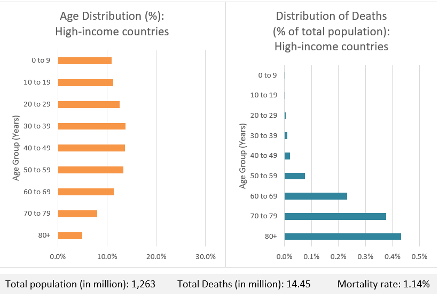
Under those assumptions, 1.3 percent of the Spanish population would be killed by the epidemic, whereas only 0.15 percent of the Ugandan population would be killed: that’s half a million fewer deaths. If we look across high-income and low-income countries broadly, the much-younger population in low-income countries would translate into a mortality rate of 0.23 percent, as opposed to a rate of 1.14 percent in high-income countries (see the figure below).
Figure. Age distribution and distribution of mortality in high- and low-income countries
Of course, almost every country is taking action to slow the spread of the virus, so hopefully the proportion of people infected will be lower. Likewise, not everyone requiring critical care will die in either high- or low-income countries. People with other health issues have higher risk of mortality from COVID-19, and people in low-income countries are at increasing risk of non-communicable diseases, as well as communicable diseases like HIV/AIDS and malaria. But the different age distribution still means that low-income countries will likely lose far fewer people to the virus than high-income countries.
What are the implications of this?
From epidemiologists, we need models of the spread of COVID-19 and the impact of different containment measures with parameters specific to low-income countries with their different age distributions, health care resources, and household sizes. The logic of “flattening the curve,” which in high-income countries relates to the capacity of intensive care beds and ventilators, needs to be theorized appropriately for a low-income context, where those medical resources are already much scarcer.
Every death is tragic, so it may seem callous to highlight this point. But in low-income countries, the increase in extreme poverty resulting from an economic slowdown will be higher, which translates into its own death toll. Moreover, in low-income countries the government’s room for fiscal stimulus and the effectiveness of monetary stimulus are much lower than high-income countries. As a result, the right balance of decisions to contain the virus versus to protect the economy may be different from that in high-income countries.
This balance has implications for the role of high-income countries in fighting COVID-19 in low-income country settings. High-income countries reap some of the benefits from low-income countries containing the virus, since COVID-19 spreads beyond borders and high-income countries have more to lose in terms of mortality. As a result, high-income countries should have an even stronger incentive to use their resources—stretched though they might be right now—to help low-income countries contain the virus and protect their vulnerable peoples and economies.
This post benefitted from research assistance by Amina Mendez Acosta and from comments by Kalipso Chalkidou, Amanda Glassman, and Mead Over.
A note on data and assumptions: For population structure, we used 2020 estimates from the UN’s World Population Prospects. The assumptions about the probability of infection and the probability of showing symptoms are from Ferguson et al. (2020), as are the age-specific estimates of the percentage of symptomatic cases requiring hospitalization and the percentage of hospitalized cases requiring critical care (Table 1).
Disclaimer
CGD blog posts reflect the views of the authors, drawing on prior research and experience in their areas of expertise. CGD is a nonpartisan, independent organization and does not take institutional positions.