Recommended

CGD NOTES
The COVID-19 pandemic caused losses of lives and livelihoods on a scale that many of us had never seen in our lifetimes, shedding light on the ways that pandemics are a “neglected dimension” of global security. And yet, as we are already observing, proposals for increased, sustained support for surveillance and preparedness are having to contend with an entrenched panic-neglect cycle in health security.
This inertia is partially the result of a variety of cognitive biases that make it difficult to grapple with low frequency, high severity events. Policymakers tend to treat epidemics as both unpredictable and inevitable, for example, assuming that COVID-19 was a “once in a lifetime” or even “once in a century” threat. This assumption—which we systematically dismantle—reduces the urgency to invest in preparedness.
This is a mistake, and potentially an extremely costly one. We propose instead a risk-informed approach to design preparedness investments, using rigorous assessments of the frequency and severity—put simply, the risk—of future epidemics. This type of process is already used to guide preparedness efforts for other natural disasters, such hurricanes and earthquakes. The time has come to apply it to the large—and rising—challenge of infectious disease threats.
A new approach to understanding epidemic risk
We’ve published new estimates of the risk of future epidemics as a joint Center for Global Development and Disease Control Priorities (DCP-4) working paper. Our approach diverges from many existing approaches in that in addition to drawing upon historical data, which is particularly suited to estimating the risk from frequent or recurring epidemics, we use a computational epidemiology framework to generate simulated data that fills in the gaps, including the crucial and data-poor region of “tail risk”—that is, infrequent, high-consequence epidemics. These types of models are very uncommon in public health literature, but widely used in other areas of natural hazard modeling, such as for floods and earthquakes.
We incorporate risk factors like zoonotic spillover, global travel patterns, and governance challenges including armed conflict. Our analysis in this working paper focuses specifically on deaths caused by epidemics of key, naturally-arising respiratory pathogens and viral hemorrhagic fevers—a subset of both the sources and consequences of epidemic risk, which represents a lower-bound estimate and not the totality of risk.
Epidemic risk is much higher than many believe
Existing methodologies have consistently underestimated the risk posed by epidemics, particularly severe epidemics. Our estimates show that in any given year, there’s a 4.2 percent probability of a respiratory pandemic causing ~10 million deaths. That amounts to a 35 percent probability in a given decade, and a 66 percent probability over a 25-year period. To put that in context, there’s a 50/50 chance—a coin flip—that another pandemic on the scale of COVID-19 will occur in the next 25 years.
Slicing the risk a different way, we can also estimate that respiratory epidemics are likely to cause, on average, about 2.5 million deaths per year. That figure is striking and may seem too high to many at first glance—and indeed, in some ways, a “typical” year would involve a substantially lower level of mortality. But part of the reason we consistently underestimate the risk of epidemics is because we fail to account for how relatively infrequent epidemics can cause massive loss of life, thus driving up our estimates of average annual loss.
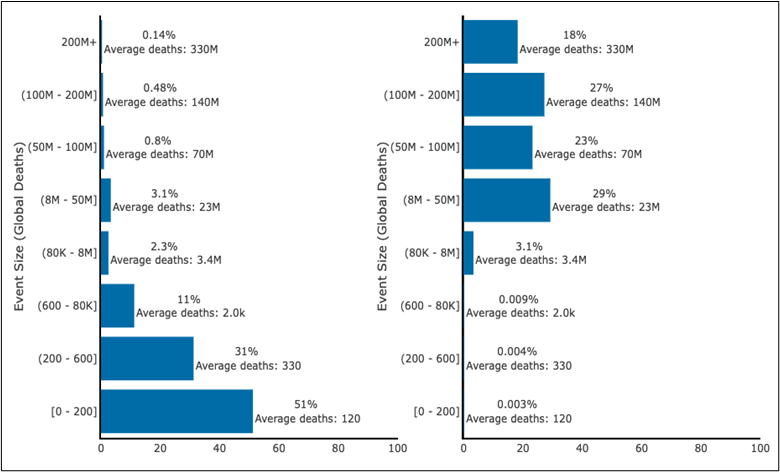
To illustrate just how skewed the distribution is, the figure below shows, based on our simulated catalog of hundreds of thousands of events, a side-by-side comparison of the risk of respiratory epidemics of varying levels of severity, with the share of total epidemics in a given period on the left, and the share of total deaths in a given period on the right. As you can see, the lion’s share of mortality is caused by severe, infrequent epidemics. Estimates that exclude this “tail risk” have a massive blind spot, motivating preparedness decisions that over-index on frequent, mild outbreaks and leave us all vulnerable to more severe events.
Figure 1: Respiratory catalog composition: simulated event sizes and their contribution to expected losses
|
Panel A: % of events |
Panel B: % of deaths |
Vulnerable populations face the greatest risk
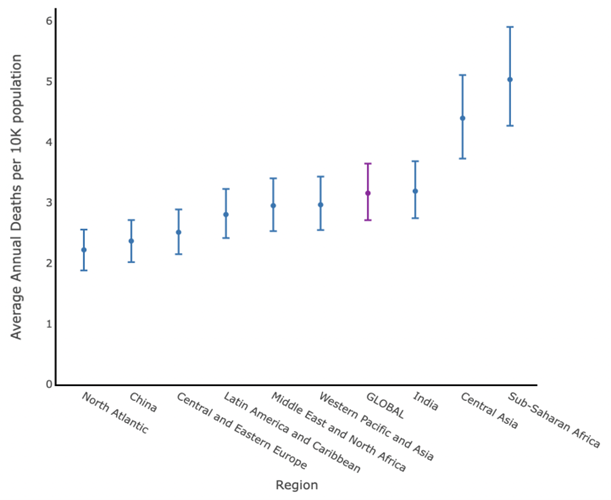
So far, we’ve been talking about global averages. But as is too often the case with global challenges, the burden of epidemics falls disproportionately on the shoulders of already vulnerable populations. From a geographic perspective, the estimated per-capita death rate from respiratory epidemics is more than twice as high in Sub-Saharan Africa than in the North Atlantic (see Figure 2 for global distribution). At first glance this estimate may seem counterintuitive, particularly given many estimates suggesting an overall lower burden of mortality from COVID-19 in Africa.
Figure 2: Average annual respiratory disease deaths, by region
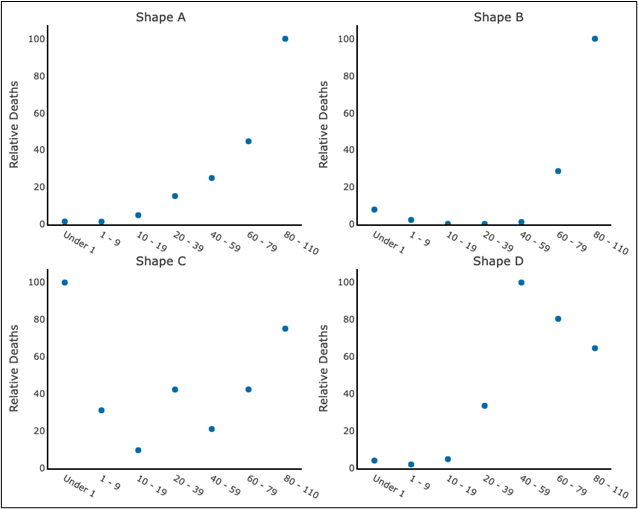
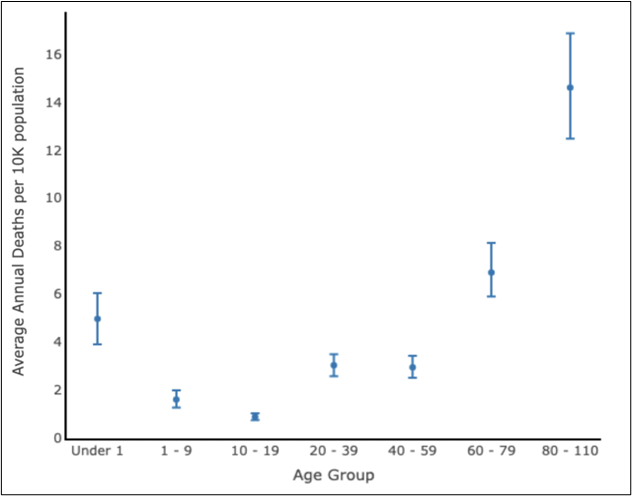
The risk in this region tends to be underestimated in part because of underreporting issues, and in part because COVID-19 was generally understood to be a disease of the old-aged. While seniors are indeed at the greatest risk of death from respiratory disease, the relative effects on different age groups can vary widely by disease (see Figure 3a). This means that overall, the risk applies not only to the oldest and youngest among us, per conventional wisdom, but also shows a more modest spike in the 20–39 and 40–59 year age groups (see Figure 3b)— a pattern that was most strikingly observed in the 1918 influenza pandemic—with concerning impacts on fertility and labor force that could ripple through the population and economy.
Figure 3a: Illustrative respiratory disease age shapes
Figure 3b: Average annual respiratory disease deaths, by age group
In addition to respiratory disease, residents of Sub-Saharan Africa also have to contend with viral hemorrhagic fevers (VHFs). VHFs are highly geographically concentrated, with 72 percent of the total global loss of life occurring in Sub-Saharan Africa alone. VHFs are expected to contribute an additional 19,000 average annual deaths in the region, with similar patterns of roughly inverse frequency and severity. VHFs are unlike respiratory diseases in that they are less likely to spread but more likely to kill those who contract them, regardless of age. This means that while the absolute risk from VHF epidemics is comparatively lower than respiratory disease, VHFs’ fatal impacts loom large for populations and policymakers in Sub-Saharan Africa.
Where do we go from here?
Our analysis is intended to provide a much-needed reality check on our understanding of epidemic risk. These estimates can be alarming and disheartening, but as we extract lessons from the hard-fought battles of the COVID-19 pandemic, we can’t afford to forget that COVID is not “once-in-a-century” risk, and moreover is only one example of the types of threats we’ll face in the coming years.
The key thing to understanding risk is that it is not immutable. An improved understanding of epidemic risk should compel us to action, to change the underlying calculus. We can reduce risk through investments in prevention, surveillance, preparedness, and response technologies and infrastructure, many of which carry broader benefits for managing endemic disease as well. And a risk-informed lens can help us allocate limited resources more efficiently, so that we direct our attention to the efforts that are most effective at keeping us safe.
We believe that rather than trying to fit epidemic risk into our existing frameworks for endemic disease, we should approach them more like natural disasters (another type of infrequent but severe event). For instance, road drainage systems and levees (infrastructure that could be directly impacted by floods) are designed with particular flood risk tolerances in mind based on local risk profiles and more general standards. What if we designed our preparedness strategies—our health systems, stockpiles, financing mechanisms, biomanufacturing facilities, and more—this way? What if we held ourselves to risk-based global standards for collective action? A risk-informed approach can help us to make better, smarter decisions, to prepare for the next pandemic.
Disclaimer
CGD blog posts reflect the views of the authors, drawing on prior research and experience in their areas of expertise. CGD is a nonpartisan, independent organization and does not take institutional positions.
Image credit for social media/web: N Felix/peopleimages.com / Adobe Stock