Recommended
Several groups have modeled the impact of COVID-19, and strategies to slow or halt its spread, on infections and deaths, including Imperial College London and the London School of Hygiene & Tropical Medicine. While their specific predictions vary based on data, policy assumptions, and modeling scenarios, they all paint a grim picture on the number of COVID-19 deaths ahead. And yet, deaths of COVID-19 patients are not the only deaths to consider when weighing up the impact of this disease, nor when assessing prospective policies or the success or failure of mitigation and suppression responses. This is the first in a series of blogs in which we’ll focus on non-COVID-19 excess deaths caused by the response to COVID-19, part of a larger project at CGD to help policymakers minimize the indirect health impacts of the pandemic.
A major gap in current models
The modeling team at Imperial predicted that an unmitigated, worst-case scenario in Africa could lead to 2,483,000 deaths, compared to 298,000 deaths in their best-case, early and sustained suppression scenario; thus 2,185,000 COVID-19 deaths could be avoided according to their predictions.
This week the medical journal BMJ Global Health published a paper authored by a team from WHO’s Regional Office for Africa. Based on more and better data, and after most countries in Africa have introduced stringent policy responses, this report predicts that between 83,000-190,000 people could die of COVID-19 in the first year of the pandemic if containment measures fail. While these new predictions are over ten times less than the Imperial projections, 190,000 excess COVID-19 deaths is a substantial toll. Still, what’s missing from these numbers are the people who will die from the many indirect impacts of the COVID-19 response.
We are not aware of any attempt to date to look across these issues to take a broader health system’s perspective. Doing so would enable us to ask, “Are stringent COVID-19 policy measures in LMICs doing more harm than good?”
Indirect consequences of the pandemic – specific disease areas
Many groups have recently begun publishing predictions of non-COVID-19 excess mortality—or what some commentators call “lockdown victims” or “collateral.” Some of their findings include:
- Using the Lives Saved Tool, Johns Hopkins University reported that across 118 low- and middle-income countries, the increase in child and maternal deaths will be devasting. Based on a range of plausible scenarios, the authors estimate that there could be as many as 2,300,000 additional child deaths and 133,000 additional maternal deaths in this first year of the pandemic as a result of unavoidable shocks, health system collapse, or intentional choices made in responding to the pandemic.
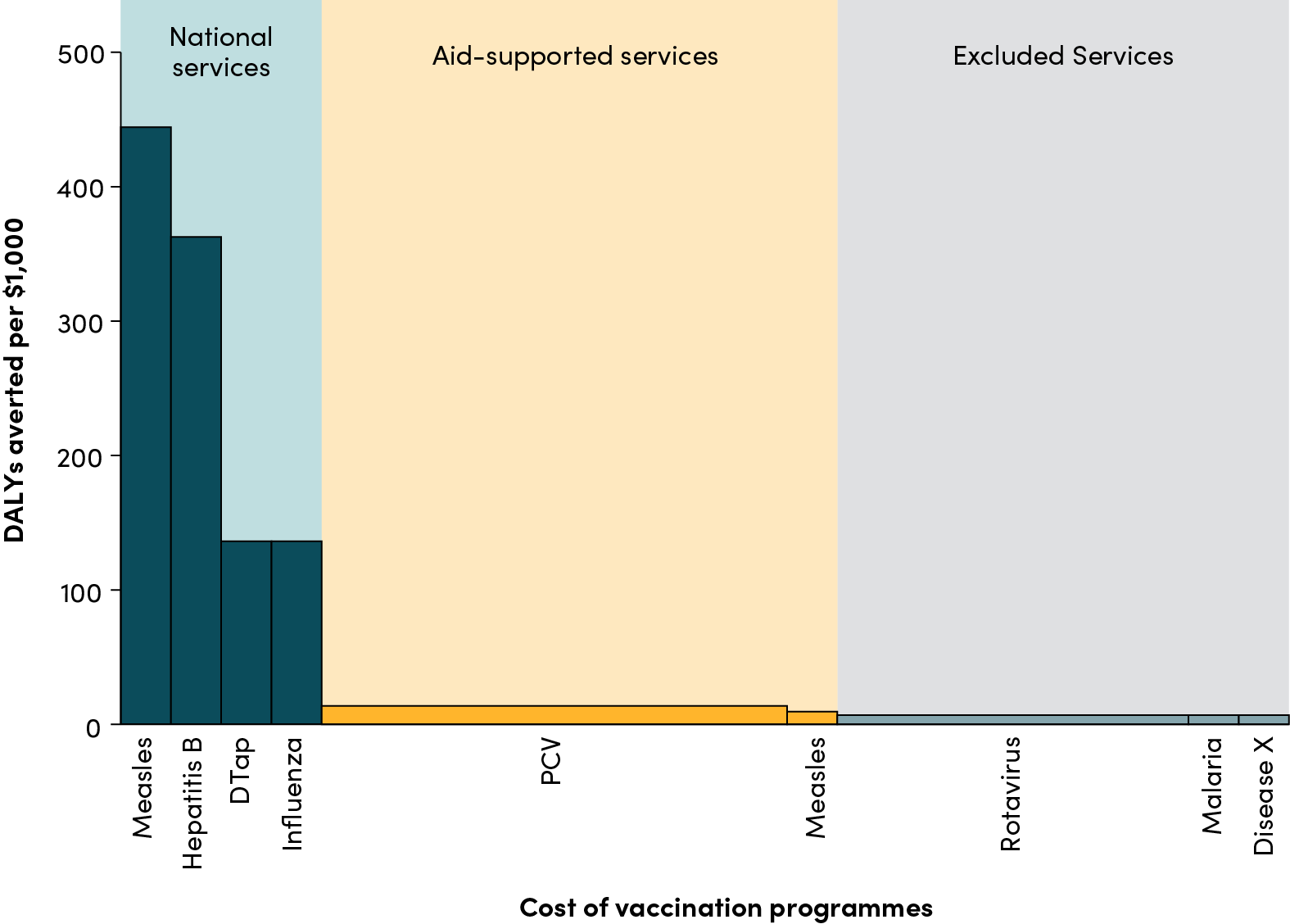
- A report by the London School of Hygiene & Tropical Medicine found that for every one excess COVID-19 death attributable to infections acquired during routine vaccination clinic visits, there could be up to 549 deaths in children prevented by sustaining routine childhood immunization in Africa. Unfortunately there are countless reports of the various ways in which the ongoing pandemic is disrupting both routine immunization and immunization campaigns.
- An HIV modelling report, convened by the WHO and UNAIDS, used five models of HIV epidemics to estimate the effect of various potential disruptions to HIV prevention and treatment services on HIV-related deaths and new infections in sub-Saharan Africa over one- and five-year periods. It found that a six-month full interruption of antiretroviral therapy (ART) supply would be expected to lead to excess deaths over a year which are more than the total current annual number of HIV deaths. In sub-Saharan Africa this amounts to possibly over additional 500,000 HIV deaths. Similar disruption would also lead to a doubling in the number of children born with HIV.
- The WHO’s Global Malaria Program considered nine scenarios for potential disruptions in access to critical malaria interventions in 41 countries. Under the worst-case scenario, in which all insecticide-treated net campaigns are suspended and there is a 75% reduction in access to effective antimalarial medicines, they reported that excess malaria deaths could approach 400,000, a more than 100 percent increase in the deaths reported in 2018.
- The Stop TB Partnership, in collaboration with the Imperial College, Avenir Health and Johns Hopkins University, estimated that a three-month lockdown and a protracted 10-month restoration could lead to an additional 1.4 million TB deaths during this time between 2020-2025.
The broader impact of COVID-19 on health systems
While these studies are useful—and we have not listed them all here—they are issue-based, with no attempt to look across the full range of essential health services that are being disrupted. Furthermore, adding up such standalone disease- and population-specific analyses could result in double-counting of excess non-COVID-19 deaths (for example maternal and child health and malaria, or child health and immunization). There has also been a conspicuous absence of modeled estimates for non-communicable diseases in low- and middle-income countries. This no doubt reflects the absence of a funded modeling consortium. By contrast, the Bill & Melinda Gates Foundation currently supports modeling consortia for HIV, TB, malaria, neglected tropical diseases, vaccines, and nutrition. However, in high-income countries such as the UK, early estimates of the cost of the policy response are emerging and seem equally devastating: a six month delay in diagnosis for new cancers could match almost half of the life-years lost due to COVID-19.
In 2017, the Global Burden of Disease project estimates that there were around 7,700,000 deaths in sub-Saharan Africa. Of these, 400,000 were from transport and other unintentional injuries. Lockdowns will result in fewer deaths from traffic accidents. Less outdoor pollution should similarly lead to less deaths, but those gains may be offset by greater exposure to indoor air pollution. But an increase of just 1-3 percent in all-cause mortality (excluding injury deaths), attributable to disruptions in the delivery of routine health services, over the course of a year, gets us to the new WHO AFRO estimates published this week: 73,000-219,000 non-COVID-19 deaths vs. 83,000-190,000 COVID-19 deaths. This back-of-an-envelope calculation should offer pause for thought, particularly as it does not consider the inevitable health effects of the global recession. Nor the effects on human capital in combination with school closures.
“An increase of just 1-3 percent in all-cause mortality (excluding injury deaths), attributable to disruptions in routine health services, would lead to the same number of non-COVID19 deaths as the new predictions of COVID-19 deaths published by WHO AFRO. This back-of-an-envelope calculation should offer us pause for thought.”
What are the alternatives?
We recognize that an unmitigated outbreak across LMICs would result in excess non-COVID-19 deaths across the whole of health due to a combination of factors including reductions in seeking care, illness and death among scarce health care workers, and overwhelming the few secondary and tertiary care facilities (a failure to “flatten the curve”). Lockdown policies will have similar consequences through disrupting supply chains, redirecting people and money to the COVID-19 response, and preventing people from seeking and accessing care. But it should not be a choice between doing nothing and lockdowns. It should be about appraising different policy options using a more holistic approach. Characterizing such excess deaths alongside lives saved from a reduction in COVID-19 transmission seems therefore to be of the essence. However, we are not aware of any attempt to date to look across these issues to take a broader health system’s perspective. Doing so would enable us to ask, “Are stringent COVID-19 policy measures in LMICs doing more harm than good?”
What is needed now
We believe that the appropriate response to this pandemic calls for nuanced, evidence-informed, and continuously refined policies. The widely modelled choice of do-nothing vs. complete shut-down is a dichotomy unhelpful to policymakers as it is both impractical in many contexts and potentially harmful, as studies are beginning to highlight. We need commonsense, context sensitive policies which openly consider the inevitable trade-offs between COVID-19 and non-COVID-19 deaths. These have been proposed and should be considered as governments plot a course through this pandemic. We list some of the suggestions in the box below, but note this list is not exhaustive.
Alternatives to total lockdown:
- Self-isolation of symptomatic people
- General physical distancing (to reduce probability of transmission per contact)
- “Looser lockdown” coupled with scaling up of COVID-19 treatment and testing capacities
- Shielding of high-risk groups (including resettlement or quarantine with limited contact and basic needs support)
- Informational interventions using phones and local/national broadcast
- Public health promotion in communities (work with local influencers, community health workers promotion of hand hygiene and respiratory etiquette)
- Special measures in informal settlements (handwashing stations, quarantine spaces)
- Regulation of high-density markets to promote physical distancing
- Local approaches to mobility restrictions (limit large scale movement, require face masks when travelling, adopt local approaches to containment)
Sources: Van Zandvoort et al., Khan and Roy, Adam et al., Inter-Agency Standing Committee
Excess deaths during the pandemic are an unintended consequences of the response to COVID-19, but they are entirely predictable based on past pandemics and other natural disasters. Estimates of the net health effects and trade-offs of non-pharmaceutical interventions ought to have informed governments’ responses including, in many countries, some of the strictest limits on movement ever seen. They are as important today to inform governments as they consider the range of policy course correction and exit options as well as responses to future waves of virus transmission.
Over the coming weeks we will share the findings of a scoping review (see here our call for resources and here for a teaser of what we’re finding) that maps data and evidence to a conceptual framework to help understand the multifaceted nature of the indirect health effects. We will also share a simple tool to support the estimation of indirect health effects, in terms of excess non-COVID-19 mortality (and also reductions in non-COVID mortality, e.g. road traffic deaths). The tool will allow users to estimate the indirect health impact across different services, and compare excess non-COVID-19 deaths as a result of COVID-19 public health measures and COVID-19 deaths averted under different scenarios. It can therefore be used to identify which non-COVID-19 services are most essential to maintain during COVID-19 to mitigate excess non-COVID-19 mortality and inform relevant policy responses. Finally, we will be launching a series of country case studies in order to document these trade-offs and will provide updates throughout this series.
Disclaimer
CGD blog posts reflect the views of the authors, drawing on prior research and experience in their areas of expertise. CGD is a nonpartisan, independent organization and does not take institutional positions.
Image credit for social media/web: Adobe Stock