by
December 01, 2009
WHO and UNAIDS have just put poor country AIDS treatment program managers on the spot. Will they choose to follow the new WHO advice to push patients to begin treatment earlier – when many are still healthy? Or will they turn their backs on the new advice and push instead for expanded access to those in need.
In conjunction with World AIDS Day on December 1, WHO and UNAIDS have released new treatment guidelines for AIDS patients. Until this week, WHO’s official position has been that AIDS treatment programs should strive to start patients on antiretroviral therapy when the number of CD4 cells in their blood drops from normal levels of between 800 and a 1,000 per cubic millimeter down to 200 per mm3. The fact that poor countries have not been able to achieve this goal accounts for WHO’s current estimate that there are about 5 million people currently needing treatment, twenty percent more than the 4 million receiving it.
There’s no question that starting treatment much later than at the 200 CD4 count endangers the patient. Studies show that patients who wait until their CD4 drops to 50 have a 50% greater mortality rate than those who start at 200. In recent years studies [e.g. here and here or here (latter requires subscription)] have shown that mortality risk can be reduced still further by starting even earlier. Now WHO is recommending that patients start ARV therapy at a CD4 count of 350, which might reduce mortality risk for the average patient by about 15%.
Should those responsible for AIDS treatment policy in poor countries respond to this advice by designing and implementing programs to identify and recruit patients much earlier, when their CD4 counts drop below the new 350 cell threshold?
In the absence of a budget constraint, the evidence of health benefits alone would be enough to argue for adopting the new policy. And for over a decade it has seemed that budgets for AIDS treatment are not constrained. But now the US government, the biggest funder of AIDS treatment, has capped its spending for the next six years to $63 billion, of which perhaps only” about $10 to $20 billion will be on treatment. As the US is expanding its war effort in Afghanistan and recovering from a deep recession, the chances of increasing this amount seem dim. AIDS policy makers need to recognize that there will be tough choices to make in this budget-constrained environment, and carefully consider the tradeoffs.
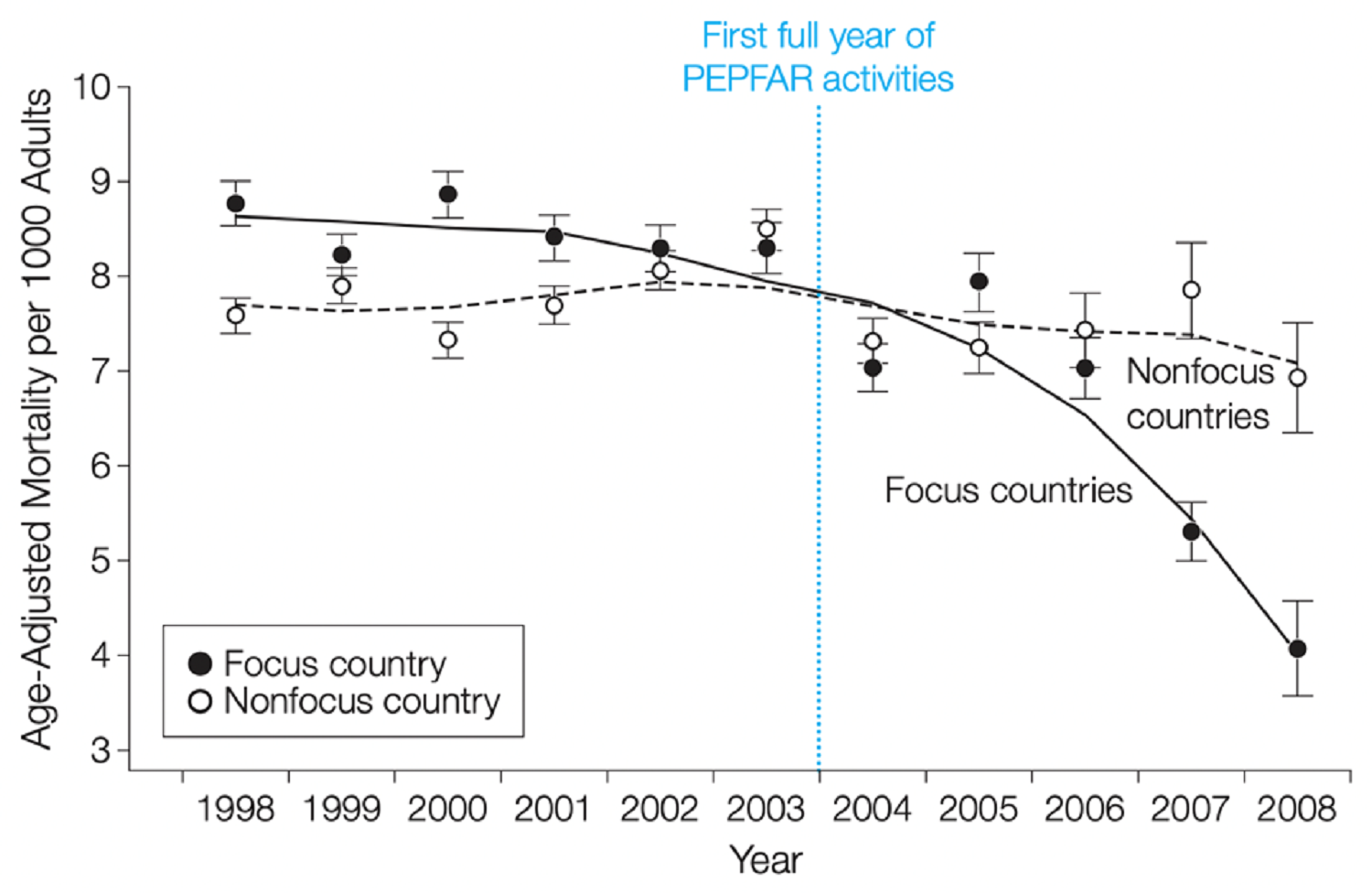
The figure below summarizes calculations that suggest the tradeoff between earlier recruitment and expanded access is stark.

Disclaimer
CGD blog posts reflect the views of the authors, drawing on prior research and experience in their areas of expertise. CGD is a nonpartisan, independent organization and does not take institutional positions.