Recommended

Event
At the Global Conference on Primary Health Care (PHC) in Astana on October 25–26, 2018, world leaders will redouble their commitment to PHC as a cornerstone of universal health coverage (UHC).[1] The event marks the 40th anniversary of the Declaration of Alma-Ata, which enshrined health as a basic human right and underscored the potential of equitable, high-quality PHC to deliver “health for all.”
There is a solid case for investing in PHC: strong PHC can, at least theoretically, meet up to 90 percent of a population’s health needs and, in turn, reduce waste from unnecessary care elsewhere in the system (Tollman et al. 2006). Moreover, investing in PHC is cost-effective and represents good value for money (Disease Control Priorities 3 2018).[2] Yet, in many low- and middle-income countries (LMICs), PHC remains under-prioritized, under-resourced, and under-utilized.
The renewed global commitment to PHC is an opportune time to distill lessons learned and identify key challenges from the past 40 years. Even more importantly, it is an opportunity to acknowledge the work that remains to be done to make vision reality.
The promise of primary health care
Since the 1978 declaration, the world has made important strides in deploying PHC services to improve health outcomes. Brazil’s Programa Saude da Familia, launched in 1994, and Thailand’s Universal Coverage Scheme, introduced in the early 2000s, are examples of large-scale nationally led efforts to strengthen health systems with a focus on PHC; both led to remarkable health gains (Glassman and Temin 2016). Indeed, governments the world over are acknowledging PHC as a building block of health systems and an important stepping stone to UHC. The Nigerian government, for example, recently announced a US$150 million investment in the Basic Healthcare Provision Fund, alongside support from the Global Financing Facility and the Bill and Melinda Gates Foundation (Global Financing Facility 2018).
Despite well-known success stories and high-level endorsements, the reality of PHC is complex. Almost half of the world’s population still lacks access to basic primary care services—such as family planning, antenatal care, and tuberculosis treatment—highlighting the limited, and in some cases uneven, progress made by countries (World Bank and WHO 2017). Even in Ethiopia, which has made great strides, a 2016 household survey found that only 38.5 percent of children 6-23 months of age were fully vaccinated, despite major support from UNICEF, Gavi, and other international agencies (Ethiopia DHS 2016, Gavi 2018). And as the burden of non-communicable diseases rises, already-weak primary care systems face added pressures to meet growing demands for complex and continuous care.
Moreover, expanding access is necessary but not enough; investments to improve quality of care are also vital. Poor quality of care is responsible for close to 5 million of the more than 8 million deaths from treatable conditions occurring annually in LMICs—far more than the 3.6 million deaths resulting from insufficient access (Kruk et al. 2018).
These statistics reveal where efforts have fallen short and, in turn, point to much work that remains to be done to move beyond the rhetoric of global declarations. Indeed, efforts to improve PHC must consider the unique set of challenges and complexities across different country contexts. Even just looking across country income groups highlights important variations: in low-income countries, donor financing accounts for a large share of resources for many key PHC elements; in several lower-middle-income countries, households tend to pay out-of-pocket for their health needs; and an increasing number of upper-middle income countries are adopting national health insurance schemes to cover more complex forms of care.[3] Even within countries, there are significant geographic and socioeconomic variations.
This note highlights four political economy challenges that explain why it is so hard to achieve strong PHC, with a focus on policy and implementation pitfalls that frequently go overlooked. With an eye towards the 2030 milestone, we offer ideas for country policymakers and global health funders to ensure greater equity, quality, and efficiency in PHC. While we acknowledge that the relevance of the challenges and ideas in this note may vary depending on context, we nonetheless hope they contribute to a deeper understanding of how to strengthen PHC systems going forward.
Why strong PHC is so difficult to achieve: Four underappreciated political economy challenges
Challenge 1: Competing demands within highly constrained public budgets means low PHC investment
LMIC governments face an already large and expanding menu of health technologies coupled with rapidly growing demand for health care, forcing them to make allocative tradeoffs within extremely limited budgets.
An expanding and increasingly educated “middle class” in urban areas means governments face growing citizen expectations for a wider range of health products and services. And a shift in disease burdens towards non-communicable diseases means governments are under pressure to deliver more complex health care. Unmet needs are huge, especially in lower-middle-income and low-income countries.
In India, less than 30 percent of end-stage kidney disease patients receive dialysis, while an estimated 200,000 new patients require treatment each year (BS B2B Bureau 2017). Nigeria has fewer than 40 trained radiation oncologists, who must use “obsolete or non-functional” treatment centers to address 100,000 new cancer cases per year (Unah 2017). And in low-income countries, challenges are underpinned by a lack of available technology. Senegal’s only radiation machine—bought in 1989—stopped working last year, leaving cancer patients to seek treatment in Morocco at the government’s expense (Quist-Arcton 2017).
Globally, 30 of the 36 countries with measured demand for radiotherapy but no available technology are low income and lower-middle income (Yap et al. 2016). This unmet demand for complex and costly nephrology and cancer care is increasingly present in public hospitals today, even in the poorest countries, and public pressure to cover treatment and management of these diseases with public budgets is mounting.
Ad hoc and inertial processes for budget allocation exacerbate the situation. Contrary to trends observed in OECD countries, which typically devote between 25 and 45 percent of total health expenditure to hospitals, hospitals often claim more than half of health expenditures in LMICs (Hatefi et al. 2017, 2016 OECD data). Some large middle-income countries that are moving towards UHC, like China, Brazil, and Nigeria, spend as much as 70 percent of their health budgets on hospital care (Lewis 2015). This may be explained in part by the underlying reality that people tend to seek curative and acute care for conditions that cause tangible distress, which are oftentimes treated in hospitals. If governments allocate resources in response to explicit demand, spending is naturally biased toward hospitals.
Without an intentional PHC financing and payment strategy and fair, systematic efforts to assess and address the efficiency of non-PHC spending, the prioritization of hospitals in health budgets combined with the growing demand for more complex care diverts resources away from primary care. In India, for example, dialysis has been fully subsidized under the Pradhan Mantri National Dialysis Programme since 2016, when less than two-thirds of children between the ages of 12 and 23 months were fully immunized (Government of India National Dialysis Services Programme 2017, Government of India National Family Health Survey 4 2015-2016).
The result is that PHC is often under-prioritized in public spending. Moreover, as many countries decentralize public administration, more and more public health money is subnational, but resource allocation does not necessarily trace to outcomes or impact (Glassman and Sakuma 2014). And in some low-income countries, allocation decisions are further complicated by the fact that there are simply not enough resources. In Malawi, for example, paying for full coverage of male circumcision, one of the most cost-effective interventions to improve health, would alone consume US$147 million—almost all of the available US$168 million health budget (Ochalek et al. 2018).
In high-income countries, the availability of new health technologies (medicines, devices, etc.) grew alongside public spending on health, enabling most new technologies to be accommodated within public budgets if they were deemed effective (see figure 1). In low-income and lower-middle-income countries, average public health spending per capita in 2015 was less than 1 percent of per capita health expenditure in the United States ( WHO Global Health Expenditure Database). Yet, these countries face the full set of health technologies and related patient and market pressures to cover new technologies with public monies within miniscule budgets, and often without institutional mechanisms in place to decide which technologies are best value-for-money or to negotiate prices. This—combined with the inertial or ad hoc budget allocation—can also wrap up scarce public resources in less cost-effective care.
Figure 1. Growth of new molecular entities compared to per capita health expenditure across different income levels
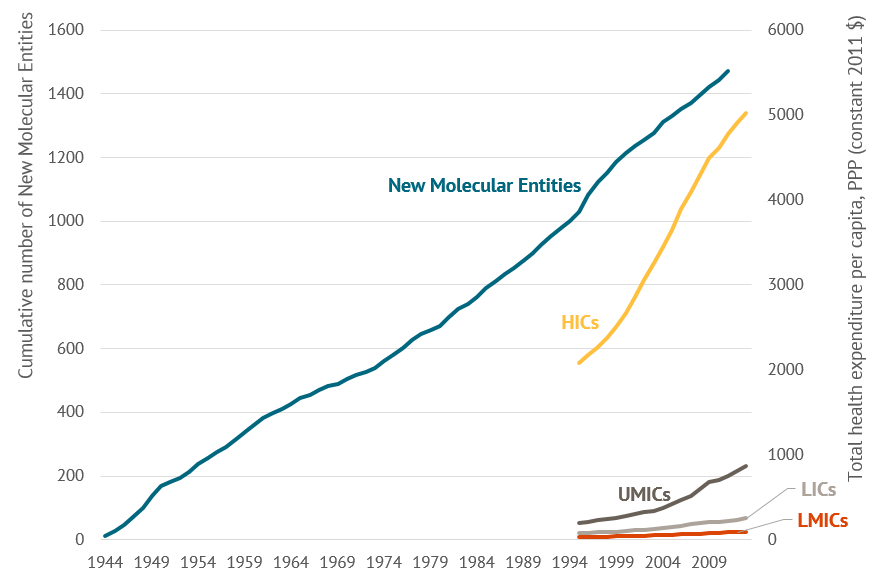
Source: Kinch et al. 2014, WHO Health Expenditure Data
Challenge 2: A vicious cycle of low productivity paired with provider absenteeism and poor quality of care results in underinvestment and underuse
Public PHC clinics in many LMIC settings simply do not produce many services due to such factors as provider absences and lack of quality infrastructure, and provide poor quality care (Kruk et al. 2018). Compounding this is the reality that families do not always seek care in public clinics, in part because of multiple cost barriers and lack of faith in the system. Instead, they oftentimes go directly to hospitals for conditions that could be addressed at the primary level, or turn to the private sector, or simply don’t seek care at all. And the way PHC clinics and teams are paid sometimes fails to create compelling incentives for greater productivity or quality, further exacerbating these challenges.
Publicly provided PHC services in many LMICs remain grossly inefficient. These inefficiencies can partly be attributed to high rates of staff absenteeism (Lewis 2006). Despite variation across and within countries, absentee rates in the public sector are staggering. In India, 40 percent of medical providers are absent in public health centers on a typical day, and in Uganda the absentee rate is as high as 50 percent (Muralidaharan et al. 2011, Chaudhury et al. 2006, World Bank Service Delivery Indicators) (see figure 2). Furthermore, many public primary care clinics see very few patients per day. In Nigeria, for example, health workers in primary health care facilities in 12 states complete less than three outpatient visits per day (Kress et al. 2016).
Poor infrastructure, including limited availability of medicines, supplies, electricity, and trained staff, is also correlated with low use of services (Kumar and Dansereau 2014). These issues are further exacerbated by the lack of professional status for primary care physicians as well as urban bias among nurses and physicians. Low productivity not only limits access and use but also adversely impacts the quality of care that people receive once they get to clinics. A survey in 18 LMICs found that, on average, consultations by primary care physicians lasted under five minutes (Irving et al. 2017).
Figure 2. Share (percent) of staff not present in public facilities
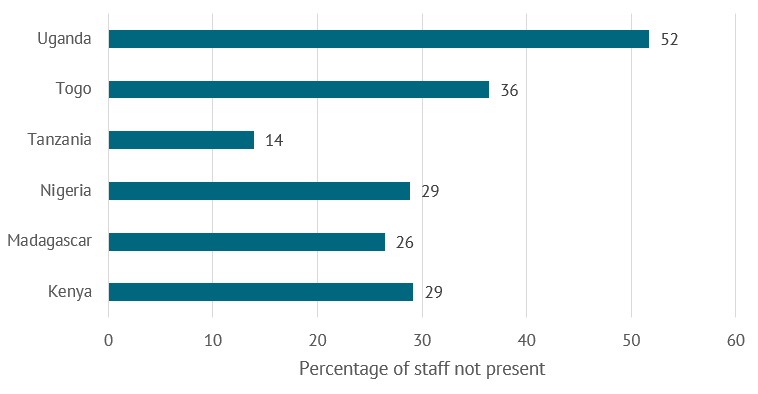
Source: World Bank Service Delivery Indicators
Notes: Absence from health facility is defined by average share of staff not in the facilities as observed during one announced visit; note that in some countries, including those shown in the figure, private clinics have similarly high levels of absenteeism. Most recent available data are as follows: Kenya (2012), Madagascar (2016), Nigeria (2013), Tanzania (2014), Togo (2013), and Uganda (2013).
A potentially reinforcing factor is that demand for primary care is disproportionately low. Families are especially less likely to seek products and services related to health promotion and disease prevention. Uptake is significantly reduced when user fees are charged for preventive health products like bed nets or deworming tablets (J-PAL Policy Insights 2018, Cohen and Dupas 2010, Kremer and Miguel 2007). Many other direct and opportunity costs also limit demand for PHC; indeed, it is common for household surveys in LMICs to report the myriad problems associated with access to care, even when a health condition is considered serious enough to merit medical care.[4] More and more evidence suggests that perceptions of low quality and lack of trust in the system lead families to bypass primary care facilities (Kruk et al. 2018).
In addition, the way incentives are structured limits the ability of primary facilities to serve as gatekeepers to the rest of the health system. For example, one pillar of India’s new Ayushman Bharat Initiative will provide poor families with health insurance, allowing beneficiaries to receive “cashless” inpatient care in both public and approved private hospitals (Kazmin 2018). While still in the early implementation stages, the scheme aims to expand access to affordable hospital services among the poor and prevent impoverishment due to catastrophic health expenditure. However, there is concern that it may incentivize beneficiaries to bypass PHC facilities and turn to hospitals (Brundtland 2018).
On the other hand, both Costa Rica and Thailand incentivize PHC providers to act as gatekeepers to the rest of the health system, referring patients to higher levels of care. Under Costa Rica’s Caja Costariciense de Suguridad Social, patients are turned back from higher levels of care if certain steps are not completed at the primary care level (OECD 2017). In Thailand, patients receive subsidized hospital care only if they are properly referred by their PHC providers (Tangcharoensathien et al. 2015). Moreover, strategic purchasing is spreading, but more work is required to understand how capitation or fee-for-service models can create incentives for better outcomes.
Together, these factors can result in a vicious cycle of low productivity and poor quality of care, which in turn results in low demand for and underinvestment in primary care.
Challenge 3: Private providers are frequently the first point of contact, but it is not always clear if and how they are part of the plan
Private providers are frequently the first point of contact in many LMICs; they can provide alternative options to low-efficiency public clinics and can potentially expand access to quality care. But, to do so they need to be effectively integrated into primary health care systems and, in many settings, public policies simply ignore the private sector or claim to regulate without adequate resources or enforcement.
Private primary care providers are oftentimes preferred over public options. In Uganda for example, 60 percent of parents with children experiencing fevers choose private sector providers as the first point of contact with the healthcare system (Buregyeye et al. 2017). Informal private providers account for around three quarters of all visits in India and Bangladesh, almost half in Nigeria, and almost a third in Kenya (The Economist 2018). Even in countries that have achieved UHC, insured patients seek care in the private sector due, in part, to poor perceptions of and low confidence in the public system’s ability to address health needs, resulting in a waste of public resources (Kruk et al. 2018).
Nonetheless, the prevalence and use of primary care providers vary across health services, countries, and socioeconomic strata. Data from 70 LMICs show that the share of services provided by the private sector may vary from 60 percent for childhood illnesses to 30 percent for family planning and 15 percent for deliveries (Grepin 2016). Another study found that the share of care sought from private providers for specific services varies drastically across LMICs from as much as 9 to 56 percent for safe deliveries to as little as 37 to 39 percent for family planning services (Campbell et al. 2016). Furthermore, use of private providers is generally more prevalent among wealthier, more educated, and urban populations, potentially exacerbating inequalities (Campbell et al. 2016, Grepin 2016).
However, rigorous empirical studies to adequately evaluate the quality of primary care across public and private providers in LMICs are few and far between, and therefore miss the opportunity to influence policy in favor of PHC-related outcomes. Two existing systematic reviews on this comparison arrive at conflicting conclusions: one suggests the private sector is marginally better in terms of drug availability and service delivery and the other finds no measurable difference. The disagreements between these two reviews can at least in part be attributed to the low quality of data in the underlying studies (Coarasa et al. 2017).
Ultimately, the ability of private providers to contribute to strong PHC systems may be shaped in large part by the institutions and policies that govern them. Indeed, there is growing acknowledgement among country governments and donors alike that partnering with the private sector and integrating private providers into national primary health care systems can help accelerate progress towards UHC. Nonetheless, doing so successfully in practice involves data and decisions on how to effectively regulate the private sector to ensure equitable and quality service delivery.
Challenge 4: PHC elements are siloed and reliant on donor funds
In many low-income and lower-income country settings, PHC elements are organized “vertically” in siloes and not integrated into broader healthcare provision. In some cases, siloes can be functional, as in immunization programs where campaigns are needed to complement routine PHC. In other cases, fragmentation and stove-piped funding persist and can be dysfunctional for better PHC outcomes across the board.
Within countries, PHC elements can be siloed; each component can have its “own” investment case, national plan or strategy, set of implementers, pots of money and financial flows, and reporting structure. In low-income countries, donors may reinforce this fragmentation, often funding PHC elements individually. This is especially the case for HIV, tuberculosis, malaria, family planning, and maternal and child health. Country supply chains for basic health commodities reflect this current practice. In Senegal, supply chains are divided by at least 13 different sources of funding, and even single commodity groups such as contraceptives and HIV diagnostic tests have multiple pipelines for procurement and delivery, resulting in parallel systems and a duplication of efforts (see figure 3).
Figure 3. Fragmented supply chains in Senegal
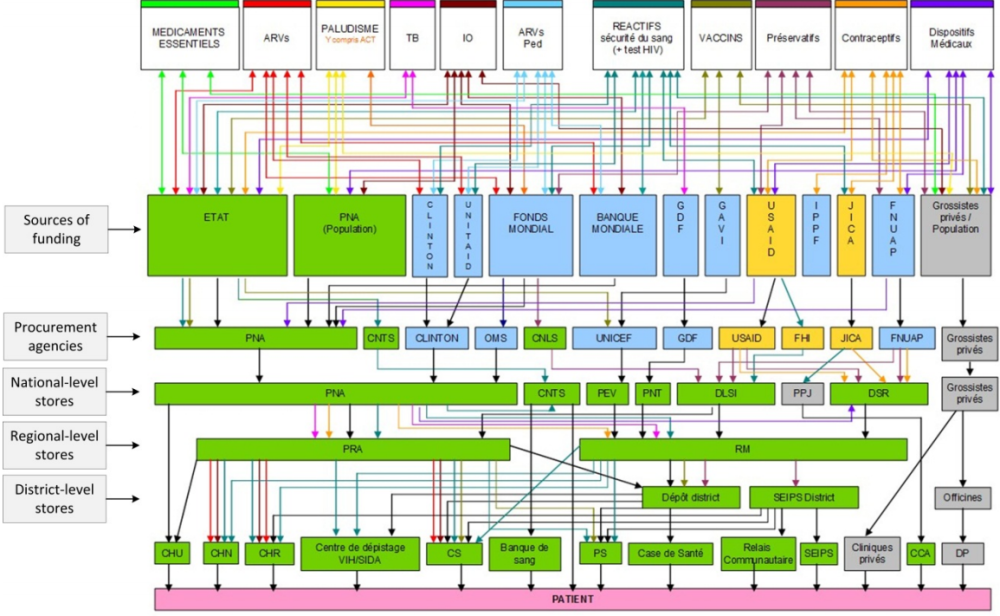
Source: Senegal Ministry of Health/Central Medical Store; cited in WHO 2013 report.
Moreover, key PHC elements in some of the poorest countries are particularly reliant on donors. Donor funding as a share of total immunization financing ranges from 60 percent in Ethiopia to nearly 90 percent in Senegal (WHO Immunization Financing Indicators, 2015). Moreover, only about a third of funding for malaria control and elimination is provided by governments of endemic countries (WHO World Malaria Report 2016). Provision of contraceptives is particularly dependent on donor support; in some low-income countries, a mere 2 percent comes from domestic resources (see figure 4).
Figure 4. Proportion of contraceptive funding by source in low-income countries
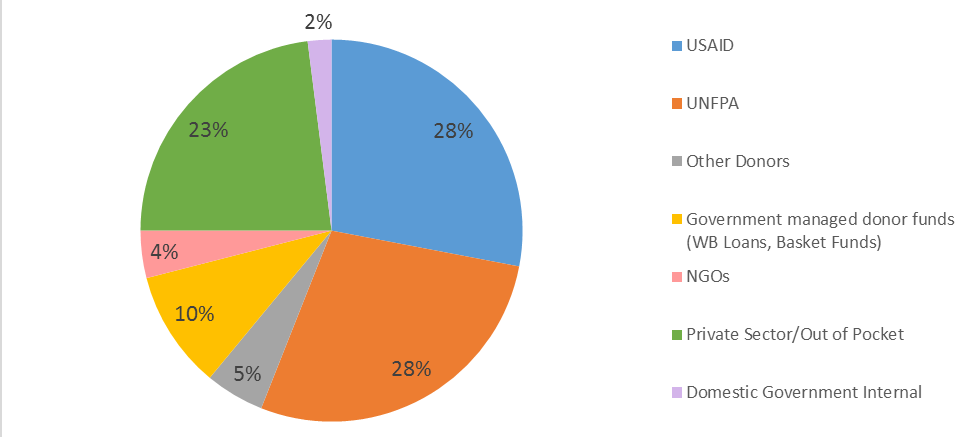
Source: Silverman 2016
The persistence of vertical siloed plans and funding makes it difficult for country governments to fully coordinate and ultimately achieve strong PHC. Tanzania is just one example where fragmentation across more than 100 distinct health information systems can stand in the way of efforts to effectively diagnose problems, ensure accountability, and drive evidence-informed improvements (Health Data Collaborative 2017). Furthermore, the sustainability of services and commodities reliant on external financing may be at risk in light of countries transitioning away from donor support. Countries are also highly vulnerable to shifting domestic priorities in donor countries that drive aid policies, particularly investments in family planning. Finally, when decentralization occurs, vertical programs can lose their funding and constituency (Williamson et al. 2014).[5]
There is growing recognition of the importance of addressing the fragmentation in global health and the need for a shift towards a systems-wide approach (Ooms et al. 2018). Indeed, integration across the health system is becoming a greater priority with calls for a “new era of global health” (Bekker et al. 2018). A strong PHC system underpinned by integrated services can be more efficient and affordable; in practice, however, this is still very much a work in progress.
From aspirations to reality: Ideas to advance better primary health care for all
We highlight below a few priority actions—by no means an exhaustive list—to help close the gaps between aspirations and reality:
- carefully consider trade-offs between alternate spending decisions
- conduct robust performance measurement and evaluation
- provide PHC where people currently seek primary care services
- put fit-for-purpose incentive structures in place
Adopt explicit resource allocation and budgeting processes with a focus on population health
Policymakers around the world must balance the needs of primary care with other levels of the health system while covering promotion, prevention, treatment, and rehabilitation all within a limited budget. Therefore, ensuring adequate resources are available to fund and staff PHC systems requires attention to the bigger picture of resource allocation and demands.
More systematic resource allocation and budgeting processes can enable governments to make evidence-based decisions about where and how to spend scarce public monies. By highlighting trade-offs between alternate spending decisions, a fair and transparent process—such as defining an explicit benefits package—can help decision makers rationalize certain investments over others (Glassman et al. 2017). Ultimately, by minimizing spending on health services and products with little evidence of cost-effectiveness, countries can get the most out of scarce resources for health.
Thailand’s Health Intervention and Technology Assessment (HITAP) stands out as one example of an evidence-based process for resource allocation. As part of the country’s Universal Coverage Scheme, HITAP systematically assesses the costs and benefits associated with including certain health services in the country’s health benefits plan. The country has achieved enormous strides in population coverage, providing a wide range of services at a low per capita budget (Glassman and Temin 2016).
At the global level, the International Decision Support Initiative, or iDSI, helps support national intuitions to drive better decisions about what a healthcare system should and should not cover, but it still operates at a small scale.[6] Systematically applying such an approach to allocation and investment decisions for primary care services is an important starting point to ensure the foundation of the health system is delivering quality, affordability, access, and equity.
Insist on rigorous, independent performance measurement and evaluation—and allocate sufficient resources for this
Rigorously and independently measuring performance is fundamental, but efforts that simply track inputs and outputs fall short; it is critical to clearly measure the outcomes of PHC that matter most: quality of care and health outcomes, including as measured by patient-recorded outcomes and patient experiences. Performance metrics together with evidence can help ensure that that resources poured into the PHC system map to measurable improvements in service coverage, quality of care, and most importantly, health outcomes.
Indeed, there is a growing body of evidence on different interventions that address the challenges underpinning PHC systems. Technological innovations, including mobile phones and other m-health interventions, have been shown to increase vaccination coverage in some contexts; overall, however, efforts have had mixed results (Farmer 2018, Oliver-Williams et al. 2017, Kazi 2017, Uddin et al. 2016). And while punitive pay-deductions or financial incentives that reward performance increase provider attendance, impacts on service utilization, quality of care, and health outcomes are similarly mixed (Huillery and Seban 2017, Ngo et al. 2017, Walque et al. 2015, Gertler and Vermeersch 2012, Banerjee et al. 2008). The bottom line: despite progress, there are still too few rigorously evaluated at-scale health programs and significant gaps remain in what we know does and does not work (Kruk et al. 2018; Glassman and Temin 2016).
It is critical to keep trying and testing different models and approaches using a wide range of assessment methods. Performance evaluations, implementation science studies, impact evaluations, and cost-effectiveness studies contribute to the different types of evidence that feed into decision making. Simply conducting more evaluations is not sufficient; these evaluations must also be of high-quality to be relevant to policy. And, sufficient investment—from donors and country governments—is paramount.
Provide PHC where people currently seek primary care services
Providing greater PHC services where people seek care can underpin a more people-centered approach. There are many possible approaches that have shown effectiveness in delivering PHC, from publicly owned and operated team care as in Brazil and South Africa, to privately owned and operated general practitioners who have contractual relationships with the rest of the health systems as in Canada and the UK, to social contracting with nongovernmental organizations to provide care.
Team-based models of community care with population empanelment and referral mechanisms to higher levels of care show promise. Brazil’s Programa Saúde da Família, for example, has provided comprehensive, cost-effective primary care services with a measurable impact on child survival and other outcomes (Glassman and Temin 2016). Although still in the early stages, results from a similar program in South Africa suggest that outreach teams can improve the overall performance of local PHC systems (Assegaai et al. 2018).
As a different approach, integrating private providers into PHC systems can improve equity and coverage and also drive increased productivity and quality. Canada’s health system, for example, has successfully integrated the private sector by administering a public universal insurance program that subsidizes PHC, which is provided in large part by the private sector and mostly through a fee-for-service model that rewards production and efficiency (Mossialos et al. 2016). In the UK, most general practitioners are private, self-employed contractors, and referrals are required for specialist care (Mossialos et al. 2016, Greenfield et al. 2016). The UK has further attempted to incentivize high-quality care from general practitioners through the Quality and Outcomes Framework (QOF), a pay-for-performance scheme that provides financial rewards for good practice as determined through set indicators. Although the framework has led to modest improvements in quality, it has significantly decreased delivery gaps (Roland and Guthrie 2016).
Other countries have contracted nongovernmental organizations to provide a package of PHC services in underserved geographical areas—experiences in countries as diverse as Afghanistan, Bangladesh, Cambodia, Guatemala, Honduras, Nicaragua, Ghana, Tanzania, and South Africa among others all stand out as successful in delivering key services and increasing coverage in some of the neediest areas across LMICs (Rao et al. 2018, Edward et al. 2011, Garcia-Prado et al. 2010, Regalia and Castro 2009, La Forgia et al. 2005, Bitran et al. 2003).
Whatever approach is taken, it is important to focus on identifying and enrolling the populations that can benefit most, and on how payment and referral work together to enable providers to manage care holistically and with a focus on patient outcomes. While we point to a number of examples, a core question is how to sustain and drive resource allocation and effort continually to PHC, whatever form it takes. Some of the private participation options may generate a constituency for PHC that would not otherwise exist.
Improve incentive structures to encourage greater domestic priority to PHC
As more and more countries face upcoming transitions from global health aid, donors must restructure their current funding to create incentives for governments to begin to sustainably fund and arrange for the rational provision of key PHC elements. One case in point is funding for family planning, particularly contraceptives, which comprise an important component of PHC. Family planning programs in countries like Nigeria and Kenya are heavily reliant on donor funding, with few incentives for co-financing. Introducing co-financing policies for family planning commodities—a strategy used by donors like Gavi—could help increase domestic spending (Silverman and Glassman 2016).
Both LMIC governments and external funders must also grapple with the reality that public monies will not come close to covering the universe of cost-effective PHC interventions and medicines. This means a persistent need for selectivity in what is covered with public monies, but also attention to enhancing the affordability of medicines and related products in the private sector, where much of health spending will persist as countries transition from middle- to high-income status.[7]
Conclusion
Failure to address these challenges head on can result in missed opportunities to drive efficiencies throughout the health system and, most importantly, to improve access to quality care and to save lives. But doing so will take much more than a global declaration; commitments backed by resources are a good start, but investments will have little impact without adequate policies and institutions to efficiently channel them to where they are most needed. Now more than ever, the global health community must adjust and adapt its approaches to protect hard-won gains and accelerate progress.
Thanks to Kalipso Chalkidou and Rachel Silverman for their feedback and thoughts.
[1] For this note, we adopt the technical definition of primary health care developed by the Primary Health Care Performance Initiative, a partnership to strengthen measurement of PHC and link data to improvements; see here for more details: http://improvingphc.org/sites/default/files/PHCPI%20Technical%20Definition%20of%20Primary%20Health%20Care.pdf.
[2] The Disease Control Priorities (third edition) found that more than half of all health interventions assessed cost less than 200 USD per DALY averted; almost all of these interventions involved treatment and prevention of basic infectious diseases, vaccinations, and basic surgical interventions, all of which are provided through PHC; see: https://openknowledge.worldbank.org/bitstream/handle/10986/28877/9781464805271.pdf?sequence=2&isAllowed=y.
[3] See here for one example of this variation in the context of purchasing for health commodities across country income groups; in low-income countries donors purchase roughly half of all health commodities; in lower-middle-income countries, the private sector is the primary purchaser of health commodities; and in upper-middle countries, the government purchases a much larger share compared to the other groups.
[4] For example, in Malawi, close to 8 out of 10 DHS respondents reported experiencing at least one barrier to care, including, but not limited to, perception that no drugs would be available or no providers would be present, distance to facility, paying for treatment; see DHS 2010 and DHS 2015-2016.
[5] For example, many countries initiating decentralization have deprioritized family planning; decentralization also fragments national family planning strategies and, in some cases, excludes stakeholders in the decision-making process. Kenya is one example where family planning and reproductive health were overlooked during recent decentralization reforms.
[6] More information is here: https://www.idsihealth.org/
[7] See Table 2 on expected health spending by source in Dieleman et al. 2017; see also this CGD note, which estimates the share of health commodities purchased by private, government, and donor/NGO financing across country income groups.
Rights & Permissions
You may use and disseminate CGD’s publications under these conditions.





