by
May 12, 2008
Last Monday, CGD posted my working paper entitled, "Prevention Failure: The Ballooning Entitlement Burden of U.S. Global AIDS Treatment Spending and What to Do About It." In response, I've received a number of e-mail comments on various aspects of the paper. A wonder of cyberspace is that I heard from far flung correspondents within hours after the working paper was posted. But the modern technology hasn't overcome the age-old problem of people interpreting an author differently than he intended. This is a chance to continue the conversation and invite others in.
One person characterizes the paper as saying that donors should "improve our efforts in prevention, and avoid ART financing." Another person feels that the title of the paper places treatment and prevention too much in competition and might lead to slower increases, if not reductions, in AIDS treatment funding. Both seem to feel that the paper exaggerates the trade-off between treatment and prevention - to the disadvantage of treatment.
In fact, I do not argue for the avoidance of ART financing, only for a clear recognition that it entails a permanent, lifetime commitment to the individual patients who receive treatment. I hope that my article helps to assure that donors who start patients on AIDS treatment in 2008 and 2009 never subsequently drop their patients for lack of budget or political will. I also urge that an increasing share of US funding for these patients be routed through multilateral institutions like the Global Fund or the development banks, in order to dilute what is otherwise an extreme form of dependency of patients and their home countries on a single donor country, namely the U.S.
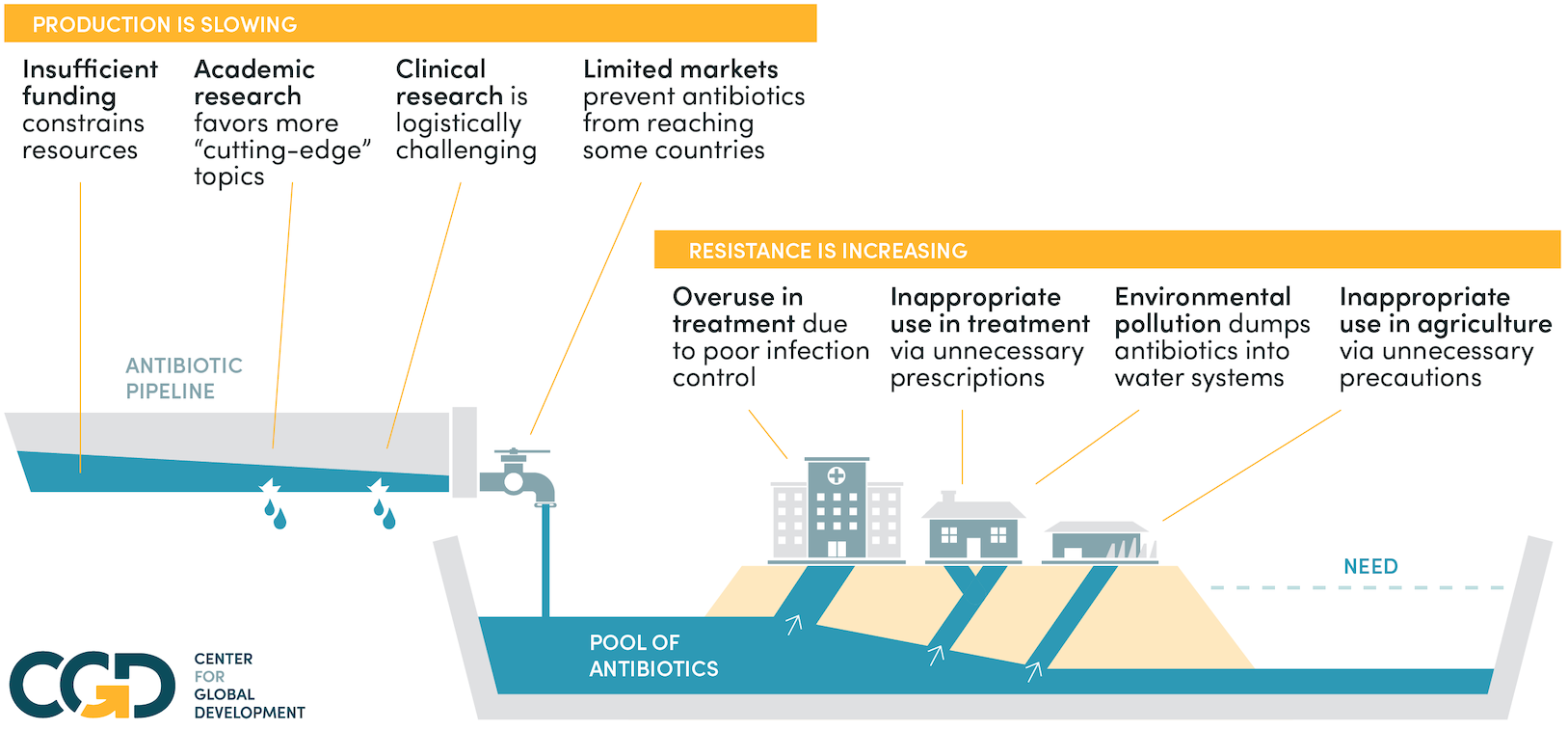
A major point of the paper is the degree to which prevention and treatment affect one another. We all know that prevention of HIV avoids the need to treat, but the article provides new estimates of the amount of treatment expenditure that could be avoided through effective prevention in PEPFAR countries.
And treatment affects prevention. Going beyond what I see as the facile assertion that treatment availability helps prevention by de-stigmatizing the disease, the paper looks at four specific types of impacts that treatment can have on prevention. These modes of interaction can be summarized in this table, which I and others have published in a book, The Economics of Effective AIDS Treatment in Thailand (Update May 14, 2008: Original table can be found on p. 78, but it has a typo which is corrected in the version presented here).
A conclusion in my paper which some people will find controversial is that the increased HIV testing stimulated by AIDS treatment availability may do more harm than good (skepticism about the efficacy of individual testing is also expressed in the just-posted article summarized here). On this point I was pleased to receive e-mail support from someone who is working on the front lines of the epidemic specifically in the area of HIV testing in Africa (she has given me permission to quote her e-mail but has asked to remain anonymous). She makes three points which add nuance to my analysis:
First she suggests that what I characterize as a shift towards provider-initiated counseling and testing (CT) is actually an expansion in that dimension rather than a shift (see Table 2 of my paper). I agree.
Second, based on her professional involvement with CT, she says:
I would agree with you that VCT [voluntary counseling and testing] remains an imperfect prevention tool and we are working on ways to strengthen the prevention component, especially for persons who test negative and continue to engage in high risk behavior.Yes, especially for them! It could turn out that the expansion of HIV testing of individuals actually increases the incidence of HIV infection rather than reducing it as suggested in the lower left cell of the above table. To improve the effect of testing on risk behavior, the solution I propose in my paper is "Couple Testing," which means that sexual partners get tested at the same time and learn each other's HIV status as well as their own. I am gratified that my correspondent says:
I completely agree with you that couples counseling needs more emphasis, both in the home and elsewhere...Let me assure you that those of us who work on counseling and HIV testing supported by PEPFAR will continue to work to expand all forms of couple counseling, not only in the home, and in traditional VCT centers, but also in "hot spots" where counseling and testing services reach out to couples in casual or non-traditional relationships...The writer's use of the term "hot spots" may be a reference to my discussion in the paper of the need to re-emphasize interventions among those with the highest risk behavior - by seeking them at "hot spots" such as bars and night clubs. I was unaware of attempts to identify and counsel sexual partners found at hot spots. This is really great news. I hope that such experiments will be thoroughly evaluated for lessons that can be applied elsewhere. Please add your comments to this blog, in order to continue the discussion on how to improve PEPFAR in years to come. If, like my correspondent, you need clearance before you can comment publicly, then fire up that old gmail account with the user name wxyz1234!
Disclaimer
CGD blog posts reflect the views of the authors, drawing on prior research and experience in their areas of expertise. CGD is a nonpartisan, independent organization and does not take institutional positions.