Recommended

Blog Post
Introduction
With many countries already facing a rising burden of disease from COVID-19, and others bracing for the looming threat, governments around the world are focused on “flattening the curve.” These efforts are critical to limit the direct health impacts of COVID-19 and to prevent already-stretched health systems from being overwhelmed. But even as the pandemic accelerates, governments must also protect other essential health services. Already, there have been numerous reports of disrupted access to services ranging from labor and delivery and immunization to HIV and tuberculosis care to dialysis and cancer treatment—most notably in countries with strict lockdowns.
Initial estimates paint a grim picture of the potential magnitude of negative impacts on health outcomes due to these disruptions. For example, real-time data from India suggests an almost 80 percent decline in daily TB notifications during the lockdown. As many as 117 million children worldwide could miss out on measles vaccinations as immunization campaigns are suspended to curb the spread of the virus. Suspension of distribution campaigns for insecticide-treated nets and disruption to malaria treatment could lead to as many as 225 million additional malaria cases across sub-Saharan Africa in 2020 alone. Further, the projected impacts for women and girls unable to access modern contraceptives, including unintended pregnancies, unsafe abortions, and maternal deaths, are staggering. Unless countries minimize the disruption of key health services, they risk facing as much if not more illness and death from the severe knock-on effects of the pandemic.
These indirect health effects are driven by supply- and demand-side factors that disrupt the provision of and access to essential health services, as our CGD colleagues recently highlighted. Supply-side barriers include supply chain interruptions of essential medicines and other health products, diversion of health resources from other services to the COVID-19 response, and paused provision of certain services to curb the spread of the virus. Demand-side obstacles include the inability of patients to access healthcare due to transport restrictions amidst lockdowns, reduced health-seeking behavior due to fear or to preserve health system capacity, and deepening poverty that may limit the ability of households to cover out-of-pocket costs.
Balancing the direct response to COVID-19 with the need for continued delivery of other health services is a universal dilemma for policymakers. But it is particularly challenging for decisionmakers in low- and middle-income countries (LMICs), where health systems already face enormous demands to address infectious and noncommunicable diseases coupled with significant capacity and resource constraints. How then should these leaders evaluate different policy options to effectively respond to COVID-19, while not exacerbating all-cause morbidity and mortality among the population from neglecting or diverting care for other conditions? And how should decision-makers explicitly acknowledge and systematically weigh the difficult trade-offs they confront? These are complex questions that merit nuanced consideration across different LMIC contexts.
This note presents an initial scoping of select trade-offs that LMIC decisionmakers and global health partners must balance across the wider spectrum of health needs as they mount a response to COVID-19. With a focus on the subset of impacts related to delivering routine healthcare, it provides examples across types of services and population groups that might be most vulnerable to the indirect effects of the pandemic and drills down on specific aspects for assessing these adverse impacts. It then highlights possible strategies for mitigation, drawing on past epidemics while noting the need to tailor approaches to LMIC settings and connect to funding sources. It concludes by underscoring the need for further research and enhanced evidence to guide response decisions that are attentive to the net health impacts over time.
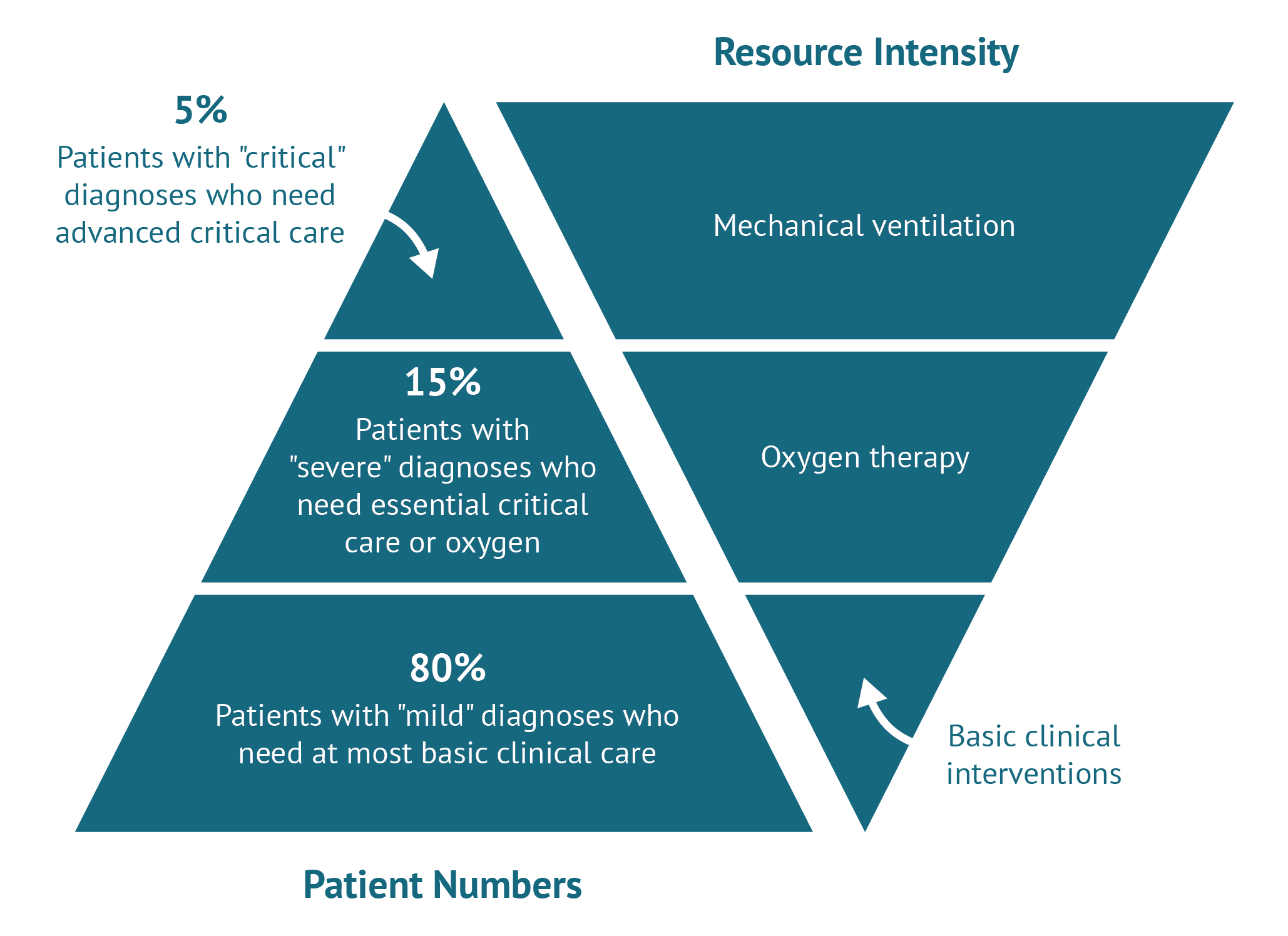
Decision-making considerations for allocating resources
As the coronavirus pandemic accelerates in LMICs, decisionmakers face particularly difficult decisions about how to allocate scarce resources—ranging from health workers and hospital beds to personal protective equipment, critical care services, and diagnostic capacity—between COVID-specific needs and other health services. Responding to the COVID-19 threat head-on is incredibly important, both to reduce direct impacts for affected patients and protect the resilience of already over-stretched health systems. Evidence also suggests COVID-19 hasdisproportionate impacts on those with underlying medical conditions, including cardiovascular disease, diabetes, respiratory illnesses like TB, and compromised immune systems related to HIV or cancer. But even if these patient groups are never exposed to the SARS-nCoV-2 virus, they are at severe risk if ongoing healthcare needs are neglected as all eyes turn to pandemic response. The nature and extent of the indirect health effects will necessarily differ by health area, population group, and underlying context. But LMIC governments, together with development partners, need to urgently account for these potentially severe knock-on effects in determining the most appropriate and feasible strategies for their populations, as our CGD colleagues have argued.
As part of their decision-making, policymakers must explicitly consider what resources might be justifiably diverted in the near term, what requires ongoing provision throughout the pandemic response, and where there may be opportunities to reduce negative consequences.
In some instances, reallocation of resources toward the response will be justified and appropriate. Indeed, countries already working with development partners can leverage existing health intervention capacities for outbreak response, as evidenced by the deployment of the polio eradication campaign’s infrastructure for surveillance and contact tracing to swiftly contain Ebola in Nigeria in 2014. Similarly, the Global Polio Eradication Initiative (GPEI) is now supporting national COVID-19 preparedness and response efforts in Nigeria, Pakistan, and Afghanistan.
On the other hand, pivoting resources and pausing services could do more harm than good. While it is difficult to generate precise estimates, evidence suggests the indirect effects of outbreak responses can be just as significant—or worse—than the direct toll of COVID-19 itself. One study estimated that a 50 percent reduction in access to services during the 2014-2015 West Africa Ebola outbreak led to an additional 10,600 deaths from malaria, HIV/AIDS and TB—almost equal to the 11,300 deaths directly caused by Ebola. While the net health impacts can be observed in the aftermath of a crisis, there are many reasons to strive for closer monitoring of adverse crowding effects in real time and build models that account for these broader health impacts across policy options. With support from development partners, national and subnational implementers must explore ways to leverage existing data sources and information feedback loops about service disruptions as the crisis unfolds (e.g., in contexts where utilization and claims data for tertiary care services may be available).
It is also critical to recognize that vulnerable groups, such as the elderly, indigenous people, those with disabilities, adolescents, and refugees and migrants, are at a heightened risk of experiencing both the direct health impacts of COVID-19 and its effects on other services. The burden will not be equally distributed across patient groups. Targeted actions and policies are necessary to protect vulnerable populations from COVID-19 and its indirect impacts.
With increasing demands on constrained public resources to address new pressures on the health system alongside the significant social and economic fallout, choices will have to be made about how to effectively meet the threat of COVID-19 and what is most critical to maintain overall health and health system resilience. WHO’s operational guidelines set out immediate actions for national, regional, and local actors to maintaining essential health services during the pandemic. But decisionmakers also need guidance on how to balance trade-offs between different response strategies, with careful consideration of the anticipated costs and consequences of diverting resources away from other high-priority health needs. This will require contextualized analyses, given different burdens of disease and levels of resource availability. For example, while pushing back non-essential procedures might be more relevant to higher-income settings, more thought is needed on what “safe de-prioritization” might look like in low-resource contexts.
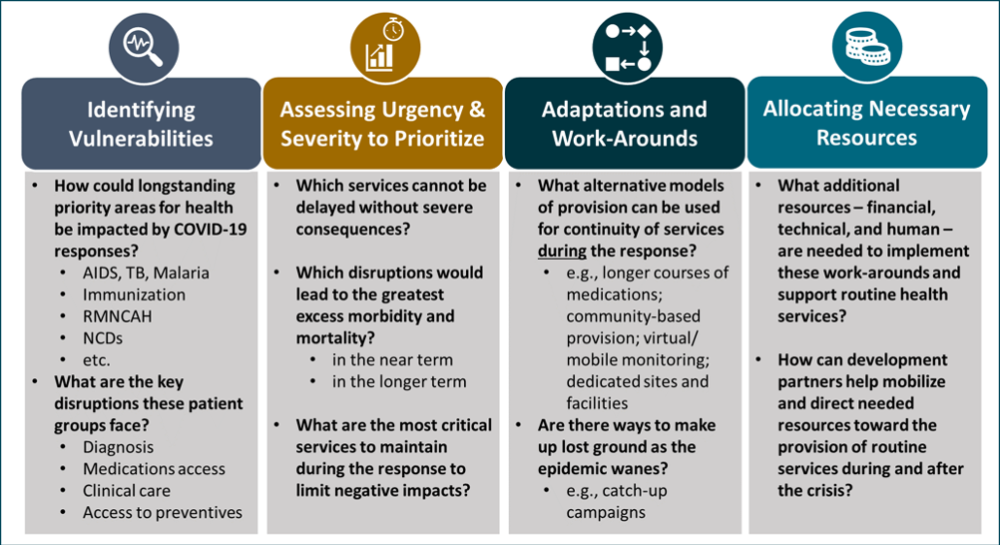
The subsequent sections of this note explore key decision-making considerations for how different response strategies may affect delivery of and access to essential health services, and what approaches could minimize adverse indirect effects (see Figure 1).
Figure 1. Key considerations for identifying and mitigating the indirect health effects of epidemics
Note: RMNCAH = Reproductive, maternal, newborn, child, and adolescent health; NCDs = non-communicable diseases.
1. Identifying key risks and vulnerabilities across other priority health areas
A detailed and contextualized assessment of what services are most at risk of disruption amidst the epidemic response—conducted with local experts familiar with the health system and appropriate technical assistance from development partners—will be a critical first step to map out reasons for disruptions, understand potential impacts of different strategies, inform decision-making to optimize response efforts, and develop plans to help mitigate the harms of COVID-19 on those with other health needs. With longstanding investments to combat the “big three” infectious disease burdens, and hard-earned progress to reduce and treat infections, global health leaders are rightly concerned about the multitude of ways in which the COVID-19 epidemic and response could put hard-won gains at risk. Beyond these areas, we will also see disruptions to critical services ranging from reproductive, maternal, newborn, and child health to the broader set of non-communicable diseases.
It will also be important to assess how disruptions at different points along the care continuum will affect near- and longer-term health outcomes. The most immediately observable indirect effects will be among those requiring acute care and intervention by trained providers for conditions with high risk of mortality. If patients are unable to access timely services, whether for stroke, heart attack, or essential obstetric and newborn care, there will be corresponding excess deaths. As response efforts continue, barriers keeping patients from managing less acute but chronic conditions will start to manifest with increasing complications, from diabetes to cardiovascular conditions to HIV, particularly with disruptions in medications access that would otherwise keep these conditions well controlled. For HIV patients on antiretrovirals, interruption to treatment poses a triple threat: increased mortality; increased transmission due to less viral suppression among those already on treatment; and treatment interruption potentially contributing to a rise in drug-resistant virus, jeopardizing the ongoing use of our best and most cost-effective options. At the same time, it will also be important to assess disruptions to upstream services related to prevention and screening. Delays in diagnosis will hinder access to timely and potentially lifesaving treatment, and by the time patients are identified, it may be too late to provide them with the most effective and cost-effective options.
Lastly, we know that preventive interventions are often among the best buys for health. But many highly cost-effective prevention services, like contraception, childhood vaccination, and bed net distribution, are at risk during the crisis as resources and attention are directed to the urgent threat of COVID-19. Alongside efforts to illustrate disruptions across the continuum of care, modeling groups are also working to project the impacts on key health outcomes, including projections for the number of excess deaths from AIDS, malaria, and TB due to the pandemic.
Below, we highlight some examples of potential disruptions and diversions across programmatic areas that have long been key priorities for the health sector in LMICs and among global health partners (click on the program area to read more). While this is not an exhaustive list, it helps illustrate the kinds of losses at stake and areas along the care continuum that should be considered. Engagement with experts across different programmatic areas and contexts can help identify the ways in which different response measures can create vulnerabilities or exacerbate existing ones—and what needs to be assessed when determining the potential impacts of service disruptions and mitigation strategies.
HIV, tuberculosis (TB), and malaria
Reports have already surfaced about HIV patients struggling to get antiretroviral therapy (ART) everywhere from the US, China, and India to Uganda, South Africa, and the Philippines—alongside various new approaches to help maintain access. Interrupted access to ART poses a triple threat: (1) increased mortality among people living with HIV; (2) increased transmission due to less viral suppression among those already on treatment; and (3) treatment interruption potentially contributing to a rise in drug-resistant virus, jeopardizing the ongoing use of our best and most cost-effective options. Similar concerns apply in the context of interrupted TB treatment, with high mortality rates among those with untreated disease and deep concerns about drug resistance. Beyond medications access, it will be important to anticipate and plan for inpatient services among these patient groups, with attention to the competing demand for pulmonary specialists and intensive care resources; respiratory infections (including TB) are a leading cause of hospitalization and death globally among people living with HIV.
There are also threats to the identification of new patients who need to be connected to care. A recent rapid assessment survey of national TB programs across 20 high-burden countries by the Stop TB Partnership found that nearly all countries experienced a decreases in diagnoses and case finding activities, with India reporting an 80 percent decrease in daily TB notifications. While the existing lab capacity for addressing the ongoing burdens of AIDS, TB, and malaria are essential capabilities to scale up wider testing of COVID-19, there is a real risk that without supplemental inputs, new demand on lab resources will crowd out diagnostic capacity for other conditions. For instance, South Africa and India are planning to leverage existing GeneXpert machines to test for COVID-19. It will be important for all countries to assess optimal workflow and integration strategies to retain use of the platform for TB and HIV, as well as the cost of this diagnostic approach for COVID-19 versus other available tests along with the cost-effectiveness of diverting use of GeneXpert from TB to COVID-19, particularly in areas with high TB prevalence.
Prevention remains paramount throughout the COVID-19 response – both to limit preventable infections and deaths and to alleviate any extra pressure on the health system during this time. In the HIV space, maintaining progress in a number of countries rolling out wider access to PrEP could be especially important during periods of lockdown, when women and girls may be subject to increased sexual violence and exploitation and greater exposure to HIV. And while COVID-19 may not pose a large direct threat to children, the suspension of key malaria interventions could result in major upticks in under-5 mortality. Accordingly, the WHO strongly advises against outright suspension of vector control activities, like the distribution of insecticide-treated nets, and encourages continued provision of preventive therapies, such as intermittent preventive treatment in pregnancy, seasonal malaria chemoprevention, and intermittent preventive treatment in infants, to protect those as greatest risk.
Immunization
Delays in immunization services to slow the spread of COVID-19 may result in an increase in morbidity and mortality from vaccine-preventable diseases, such as measles, cholera, HPV, yellow fever, and meningitis. WHO recommends that governments temporarily halt preventive immunization campaigns, and the GPEI has paused all polio vaccination campaigns, inevitably backsliding global polio eradication efforts. The Measles & Rubella Initiative warned that 117 million children may miss out on immunization against measles. Gavi is sounding alarm bells about the implications of COVID-19 on its programs: as of early April, 14 major Gavi-supported vaccination campaigns and four national vaccine introductions were postponed, which will result in 13.5 million people missing out on vaccinations in 13 of the world’s poorest countries. This number will continue to rise as more campaigns are put on hold. As countries consider which immunization strategies should be sustained or paused, they must assess the gains in reducing transmission against the cost of leaving key populations unprotected from other vaccine-preventable disease threats. One recent study examining risks and benefits of sustaining routine immunization services in Africa found that for one excess COVID-19 death attributable to infection at service delivery points, approximately 101 future deaths would be prevented in children through to age 5 years by continuing vaccination programs.
The projected harms of pausing different vaccination campaigns will vary by context based on the existing pockets of disease, baseline coverage rates of immunization and herd effects, seasonality of a particular threat, and other transmission dynamics that may be influenced by aspects of the COVID pandemic (e.g., rapid movement of populations to evade travel bans, further overcrowding in informal settlements amidst lockdowns). In some cases, there may be appropriate pauses on certain immunization activities, particularly when the threat of a delay seems minimal and there is potential to make up ground on coverage after the major threat of COVID-19 abates. For instance, pausing HPV vaccinations, which are often administered through school-based programs, would not pose an immediate threat to those unvaccinated at the time since they are typically targeted to girls ahead of sexual debut to prevent cervical cancer several years down the road. There would still be a relatively large window of time to reach at-risk girls through future immunization activities, even if this would require adjusted eligibility to school-based programs and/or strategic catch-up campaigns.
Reproductive, maternal, newborn, child, and adolescent health (RMNCAH)
Globally, around 200 million women are pregnant each year, 90 million give birth in health facilities, and another 700 million rely on access to modern contraceptive methods. While tremendous progress has been made in recent decades in expanding coverage of essential sexual and reproductive health services, with significant reductions in maternal and newborn deaths as well as unintended pregnancies, service disruptions during the COVID-19 response pose major threats to these gains. It may seem obvious that pregnant women will need labor and delivery services; after all, this is not a service that can be delayed or deprioritized. But there have already been reports from several countries, including China, Ethiopia, and Uganda, about the challenges pregnant women face in accessing services with disruptions to transport, lockdowns, and diverted health staff. Within care settings, there may be additional constraints on or shocks to the supply of essential goods for emergency obstetrical care, such as adequate blood supply to respond to post-partum hemorrhage. Without concerted efforts, we are likely to witness disruptions along the entire care continuum, from contraceptive access and safe abortion services, to essential antenatal care (including HIV screening and preventing mother-to-child transmission), through labor and delivery and postnatal care. Case in point: outreach services for RMNCAH have been halted in several states in India that already have the highest maternal and infant mortality rates.
The Guttmacher Institute estimated that a 10 percent reduction in service coverage of essential pregnancy-related and newborn care and contraceptive use could respectively result in an additional 28,000 maternal deaths, 168,000 newborn deaths, millions of major obstetric and newborn complications, and over 15 million unintended pregnancies. And based on previous epidemics, a 10 percent decline in RMNCAH services may be a stark underestimation of potential disruption. During the Ebola outbreak, for example, deliveries in health facilities decreased by 30 percent.
Many international organizations have expressed concerns about the consequences of lockdowns on safe abortion access, let alone politicized moves to deem the procedure nonessential during the response, despite the time-sensitivity of pregnancy termination. In addition, supply chain disruptions will likely generate shortages of contraceptive commodities and medications to treat sexually transmitted infections. DKT, a family planning service provider, has already reported stockouts of implants in Myanmar and an anticipated condom shortage in Mozambique due to doubling delivery times from manufacturers. (Stay tuned for more from CGD on addressing shortages of non-COVID medical supplies.)
Non-communicable diseases (NCDs)
The rising rates in LMICs of cardiovascular diseases, cancers, diabetes, chronic lung diseases, and other NCDs have garnered significant attention, including how to meet the growing needs of these patients alongside the longstanding focus on infectious disease threats. The COVID-19 pandemic poses a double threat to patients with these conditions, given the increased risk of severe disease they face if infected and the indirect harm of care disruption to manage their chronic disease. In India, there have been reports of police stopping dialysis patients from traveling to their appointments, while in China, cancer patients have been turned away from chemotherapy and emergency surgery, finding that “there are no resources left for patients who don’t have the virus.” There are also significant concerns that people with acute conditions, such strokes and heart attacks, are avoiding seeking timely care out of fear of exposure to the virus or in response to messaging about reducing burden on health system capacity; many health systems are reporting significant decreases in cardiovascular and other services. Pauses in cancer services such as screening programs and delays in early stage interventions may very well contribute to excess mortality and higher costs to address more advanced cancer cases.
Policymakers must carefully weigh changes in service provision for NCD prevention and care to assess how disruptions will contribute to excess mortality, disease burden, and downstream healthcare costs. For example, India’s largest cancer center is using a proactive and multipronged approach to carefully and intentionally scale back some services in order to maintain other routine care. Lastly, there may also be opportunities to assess how to better address unmet needs for mental health in the context of COVID, as treatment gaps and burdens are expected to worsen due to anxiety, depression, and stress from social isolation, fear, and loss.
2. Evaluating the nature, magnitude, and distribution of consequences to different priority health services and sub-populations
The nature of the risks to other health areas can be quite varied, with some concentrated among the existing patient population and others posing wider threats surrounding community transmission of disease and rises in drug-resistant pathogens. For certain services, there may be some leeway to pause or delay provision and make up ground later when the threat of COVID-19 is not as great. But other service interruptions will result in dramatic increases in morbidity and mortality in the near and longer term—with serious backsliding on major areas of progress in global health gains that cannot easily be recovered. As noted earlier, the greatest harms are likely to be to those already disadvantaged: the marginalized, vulnerable, and poor.
This underscores the importance of evaluating and quantifying the impacts of various response measures, mitigation tactics, and resource reallocations, using the best available data to inform or model the potential cumulative health impacts and distribution of harms and benefits across populations groups facing different health threats. Various efforts are now being explored to leverage modelling expertise in service of better decision-making for health in the face of COVID-19, including what is appropriate for LMICs given existing disease burdens and constrained resources. For example, assessing the COVID-19 specific benefits of pausing childhood immunization services against the significantly higher benefits of sustaining vaccinations for children under 5 illustrates the importance of quantifying comparative health impacts when making decisions about service provision.
As new analytical tools are deployed to guide evidence-informed decision-making, the following should be made explicit to policymakers assessing the various trade-offs:
Risks of death, disability, or long-term morbidity as a result of service disruptions—with attention to the urgency required to avert negative health outcomes
Risks of wider community transmission of other infectious diseases, for instance with paused immunizations or reduced viral suppression of HIV
Distribution of these impacts across segments of the population (including by age, gender, geography, socioeconomic status, etc.)
Consequences for available treatment options (e.g., if interruptions could lead to resistance to first line, cost-effective options; how delays in access to some therapies may mean they are less effective in treating more advanced disease)
Longer-term impacts on the health system when the threat of COVID-19 abates
The last category includes the potential impacts of options on the health workforce itself, recognizing frontline workers as a critical resource to meet all health needs. Because health workers face increasing exposure and mortality from infectious disease threats, the loss of these providers can have long-lasting downstream health impacts for a country and its people.
Evans et al. (2015) explored the secondary effects of healthcare worker deaths during the West Africa Ebola outbreak on maternal, infant, and child health outcomes, and identified significant knock-on effects for maternal mortality across Guinea, Liberia, and Sierra Leone. Their work highlights the role that limiting nonessential services can have in reducing health worker exposures while reserving much-needed personal protective equipment for health workers offering critical services. At the same time, any pause in services deemed nonessential during the response requires consideration of built-up demand and the risk that delayed presentation of patients with more advanced disease could be costlier and further strain health systems and providers when services resume.
Given that any models used to prospectively evaluate these impacts will rely on imperfect information and numerous assumptions, ongoing data collection efforts (and use of real-time data, to the extent possible) should inform updated assessments of adverse impacts and needed course corrections as the pandemic response evolves.
3. Adaptive strategies and workarounds to deliver key services and mitigate harmful impacts of COVID-19 on other health priorities
Many governments, alongside development partners and local civil society organizations, have been exploring feasible work-around strategies to help meet the needs of those whose health needs have been indirectly impacted by the pandemic. Below we summarize some solutions that have been deployed in the current context or in past epidemic responses that should be considered. Of course, these types of solutions have to be explored with appropriateness and feasibility in a given context. And some of these strategies might still fall short of ensuring continued access to the most vulnerable groups.
Medication delivery and dispensing: There has been wide recognition of the value of enabling access to longer courses of medications and multi-month refills, particularly among HIV and TB programs, with many countries adopting new policies for extended prescriptions and multi-month dispensing of ARVs. WHO and PEPFAR have recommended providing up to a 6-month supply of ARVs to people living with HIV and the Global Fund has advised a 3-6 month supply and is helping to supplement emergency stocks of medications in various countries. Home delivery of ARVs to reach those with limited access has also been deployed in the Philippines and the Republic of Moldova, enabled through partnerships with NGOs and civil society organizations. There have been similar calls for multi-month dispensing and delivery of other essential medications, including contraceptives, medical abortion pills, and drugs to manage other chronic diseases like diabetes and heart disease. However, disruptions in the supply chain alongside spikes in near-term demand may present challenges to wider implementation of this strategy, and the successful roll-out will likely require a combination of regulatory changes, international coordination, and support from development partners, and local collaboration with NGOs to facilitate access and delivery. The Global Fund and Stop TB Partnership have also flagged the need to monitor adherence and adverse events for home-based TB care, and the latter recently put out a note on available resources to support virtual care and community-based monitoring.
Community-based care: In many settings, community health work already forms the backbone for primary health provision. In the context of COVID-19, the use of community health workers, health extension workers, and other technologies that facilitate home-based care present important opportunities to continue providing services outside healthcare facilities while appropriately triaging and referring people with more acute needs to higher-level care. For example, during the Ebola outbreak, community actors were engaged late in the response, but were eventually able to promote antenatal care, help women plan for facility-based deliveries, and provide or connect them to family planning services. In India, frontline health workers have already been tasked with communication, education, and referral services for COVID-19, complicating their efforts to maintain routine service delivery. As is always the case, successful deployment of community actors will require formal engagement, support, and adequate information and resources. Encouragingly, Merck for Mothers has pledged $3 million to help health systems better meet the needs of pregnant women before, during, and following delivery while tackling COVID-19, with specific investments to be determined. But increasing reliance on community provision of services to meet various health needs outside of facilities will require sufficient fiscal and technical support.
Dedicated treatment spaces: Various technical guidance pieces have highlighted the role for dedicated clinic spaces for COVID-19 patients to reduce exposure risks among already vulnerable patient groups and help allay fears about seeking needed services during this crisis. For instance, PEPFAR advised setting up dedicated HIV clinic spaces where they do not already exist, and UNFPA recommended antenatal and postnatal care facilities and/or mobile clinics to support the continuum of maternal and newborn care. Various countries have also been establishing dedicated COVID treatment centers for mild cases or even entirely new hospitals to preserve existing clinical capacity to meet other health needs. However, dedicated COVID treatment or step-down facilities may only prove useful if the overall number of cases are kept to a manageable volume. Any reorganization or enhancement of clinic spaces would need to be supplemented with clear communication so people know where to access services, as well as appropriate screening, triage, and infection prevention and control strategies to reduce the chance of introducing COVID-19 in care settings for other conditions that may be high-risk comorbidities.
mHealth, digital tools and ICT solutions: the use of digital technologies to improve health in LMIC settings has been a rich space for experimentation and innovation long before COVID-19. With increasing penetration of mobile phone ownership, mHealth tools not only provide novel ways to track the impacts of COVID, but also to disseminate information, mobile money, and provide assistance for managing various health conditions during social distancing periods. Exploring available tools and platforms that can be leveraged across different programmatic areas for various aspects of care provision and communication—and assessing which populations will and will not be reached through these solutions—may offer strategic ways to remotely manage certain health needs during periods of the response. For example, the Stop TB partnership has compiled a list of digital technology solutions that may be particularly useful for tuberculosis programs and patients during this crisis. Use of these technologies must also take account of various privacy and confidentiality concerns, with appropriate safeguards, while also recognizing the limitations of these approaches in reaching the most vulnerable who do not have adequate access to phones, devices, and network connectivity. Investing in health data innovations and telemedicine, alongside facility and infrastructure upgrades, could be impactful ways for development finance institutions to contribute to the COVID-19 response.
This is in no way an exhaustive list of possible solutions, strategies, and work-arounds. For instance, there will be a clear role for supplemental immunization activities and catch-up campaigns to reach populations missed during the pandemic response (e.g., for paused polio and HPV vaccinations as well as other immunizations with lower uptake). Other innovations will be needed to address challenges during COVID-19 responses, such as disruptions to transportation and deepening levels of food insecurity and malnutrition, which have cross-cutting impacts on nearly all health conditions. There may be scope to leverage recent innovations, like those addressing emergency transport in Kenya. Efforts to provide outreach services for those hit hardest by disruptions in health services, food access, and transit may benefit from joint provision or linkages between programmatic offerings. For a comprehensive list of novel approaches, Global Innovation Exchange’s COVID-19 Innovation Hub highlights relevant innovations across 12 categories, including transportation, emergency communications, data, and vulnerable groups.
4. Mobilizing resources to support service continuity and adaptations, evidence-informed prioritization, and post-COVID recovery efforts
Generating the necessary evidence to inform response strategies and augmenting activities to sustain access to essential health services during the crisis will require substantial resources. Development partners focused on global health have an important role to play in supporting countries with technical guidance on how to prioritize and design context-appropriate strategies to protect non-COVID healthcare programs during the pandemic, along with providing financial support during and after the crisis. Encouragingly, many global health funders have adapted quickly to support recipient countries. To help address COVID-19, and with an eye towards resuming immunization services after lockdown measures subside, Gavi has committed up to $200 million to help lower-income countries respond. As part of this commitment, countries can reallocate up to 10 percent of grants from Gavi’s health system and immunization strengthening program to address COVID-19. Continued support from Gavi during the pandemic and beyond will also be critical to cover lost ground. Similarly, the Global Fund is providing up to $1 billion in grant flexibilities and additional support for country responses to the pandemic and “continuity in the fight against HIV, TB and malaria.” And PEPFAR is working to provide country and regional teams with greater flexibility to serve HIV patients in local contexts affected by COVID-19 while also leveraging its laboratory capacity and surveillance systems to support COVID-19 diagnostics.
Questions remain about how new monies and aid reallocations will be programmed by multilateral and bilateral donors going forward. While the crisis calls for as much flexibility and speed in financing as possible, global health funders will have to strategically balance their specific remits with broader outbreak response efforts to avoid diverting resources away from their focus areas and prevent backsliding. Further, increasing fiscal uncertainties in both LMIC settings and donor countries due to the economic consequences of the pandemic, including reduced government revenues and rising debt levels, will further mire financing challenges. One telling example: reports suggest France may be reallocating aid monies for Africa to focus on its response at home. While the need for external support in LMICs has never been greater, uncertainties in the future of the global health donor landscape risk further constraining LMIC resources.
The need for enhanced evidence and research to guide decision-making
Ultimately, decisionmakers must acknowledge that not every need can be met. Even with innovative strategies and additional resources, some services will need to be deprioritized as part of the response. Unfortunately, policymakers currently lack rigorous data on the indirect health implications of reallocated resources. (Equally worrisome, some have little visibility into the direct health impacts and costs of COVID-targeted interventions; data on their comparative cost-effectiveness thus far is mainly applicable to high-income countries, with limited engagement and access for LMIC policymakers.) As the pandemic spreads to LMICs, decisionmakers will require better data and evidence, well-adapted modelling tools, and nuanced guidance to balance local responses to the immediate effects of COVID-19 with protecting essential health services.
The outlined challenges for decision-making and resource allocation, vulnerabilities to specific health areas, and proposed mitigation strategies underscore the need for policymakers and the broader global health community to carefully consider the costs of overlooking other high-priority health needs. Whatever strategies are pursued to simultaneously meet the COVID-19 threat alongside other health needs, transparency and effective communication will be critical. Policymakers will need to be attentive to clear communication about why they are pursuing their adopted approaches, which services remain available and through what channels to ensure appropriate uptake, allaying fears about care-seeking, and combatting misinformation. It will also be imperative to facilitate ongoing data collection on the indirect health impacts of COVID-19 across the health sector and evaluate the effectiveness of adaptive strategies – not just to inform and course correct during the current crisis but to build the evidence base for efforts in future epidemics and longer-term health system capacity building.
Over the coming months, CGD colleagues will be conducting an in-depth assessment of the knock-on effects of COVID-19 on access and provision of healthcare services, particularly in LMICs, with the goal to inform decisions and develop pragmatic approaches to mitigate these effects. As part of ongoing scoping efforts, our colleagues recently put out an open call for reports and data on how COVID-19 is impacting health services for other conditions. As this work progresses, CGD aims to build a public repository documenting these accounts and relevant research as a resource for policymakers, alongside case studies and additional analyses and tools to more systematically consider the tradeoffs and net health impacts of outbreak containment strategies. Stay tuned for upcoming work.
Rights & Permissions
You may use and disseminate CGD’s publications under these conditions.